
- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.


14.3: Structures of the Male Reproductive System
- Last updated
- Save as PDF
- Page ID 30720

- Suzanne Wakim & Mandeep Grewal
- Butte College
Rocky Mountain Oysters
First, they are peeled and pounded flat. Then, they are coated in flour, seasoned with salt and pepper, and deep-fried. What are they? They are often called Rocky Mountain oysters, but they don’t come from the sea. They may also be known as Montana tendergroin, cowboy caviar, or swinging beef — all names that hint at their origins. Here’s another hint: they are harvested only from male animals, such as bulls or sheep. What are they? In a word: testes.

Testes and Scrotum
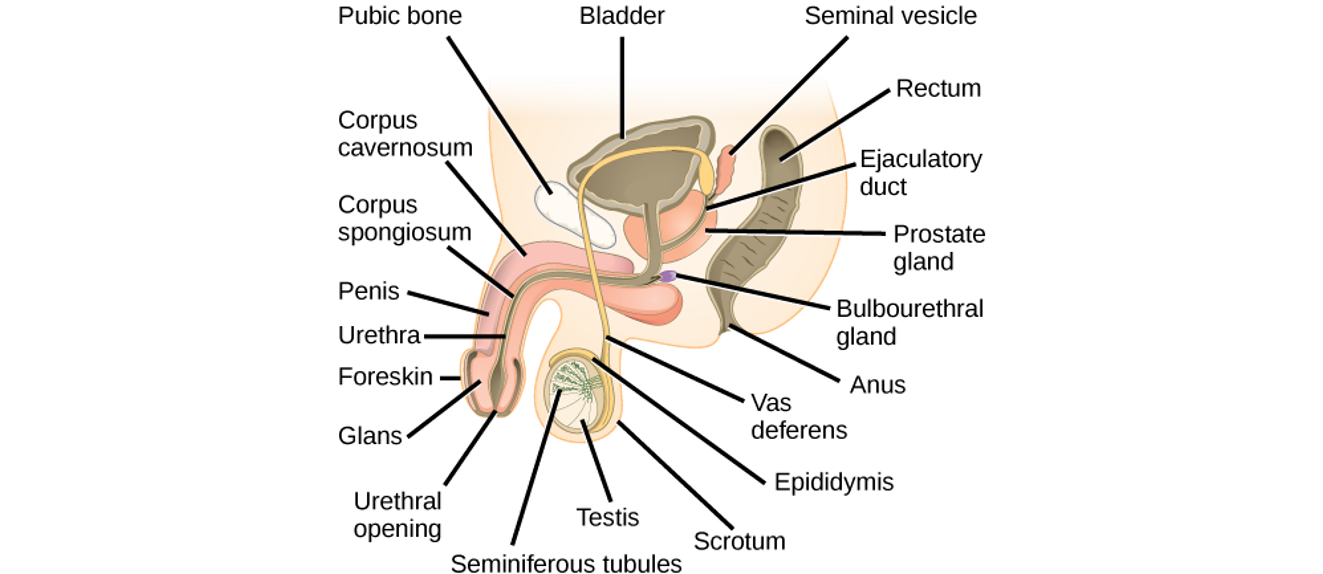
The two testes (singular, testis) are sperm- and testosterone-producing gonads in male mammals, including male humans. These and other organs of the human male reproductive system are shown in Figure \(\PageIndex{2}\). The testes are contained within the scrotum, a pouch made of skin and smooth muscle that hangs down behind the penis.
Testes Structure

The testes are filled with hundreds of tiny tubes, called seminiferous tubules , which are the functional units of the testes. The seminiferous tubules are coiled and tightly packed within divisions of the testis called lobules. Lobules are separated from one another by internal walls (or septa).
One or more seminiferous tubules are tightly coiled within each of the hundreds of lobules in the testis. A single testis normally contains a total of about 30 m (90 ft) of these tightly packed tubules! As shown in the cross-sectional drawing of a seminiferous tubule in Figure \(\PageIndex{2}\), the tubule contains sperm in several different stages of development
Other Scrotal Structures
Besides the two testes, the scrotum also contains a pair of organs called epididymes (singular, epididymis) and part of each of the paired vas deferens (or ducti deferens). Both structures play important functions in the production or transport of sperm.
The seminiferous tubules within each testis join together to form ducts (called efferent ducts) that transport immature sperm to the epididymis associated with that testis. Each epididymis (plural, epididymes) consists of a tightly coiled tubule with a total length of about 6 m (20 ft). As shown in Figure \(\PageIndex{2}\) the epididymis is generally divided into three parts: the head (which rests on top of the testis), the body (which drapes down the side of the testis), and the tail (which joins with the vas deferens near the bottom of the testis). The functions of the two epididymes are to mature sperm, and then to store that mature sperm until they leave the body during an ejaculation when they pass the sperm on to the vas deferens.
Vas Deferens
The vas deferens, also known as sperm ducts, are a pair of thin tubes, each about 30 cm (1 ft) long, which begin at the epididymis in the scrotum and continue up into the pelvic cavity. They are composed of ciliated epithelium and smooth muscle. These structures help the vas deferens fulfill their function of transporting sperm from the epididymes to the ejaculatory ducts, which are accessory structures of the male reproductive system.
Accessory Structures
In addition to the structures within the scrotum, the male reproductive system includes several internal accessory structures. They include the ejaculatory ducts, seminal vesicles, and the prostate and bulbourethral (Cowper’s) glands. See Figure \(\PageIndex{3}\). The major reproductive structures represented in this figure are explained below.
Seminal Vesicles
The seminal vesicles are a pair of glands that each consist of a single tube, which is folded and coiled upon itself. Each vesicle is about 5 cm (2 in.) long and has an excretory duct that merges with the vas deferens to form one of the two ejaculatory ducts. Fluid secreted by the seminal vesicles into the ducts makes up about 70 percent of the total volume of semen, which is the sperm-containing fluid that leaves the penis during an ejaculation. The fluid from the seminal vesicles is alkaline, so it gives semen a basic pH that helps prolong the lifespan of sperm after it enters the acidic secretions inside the female vagina. Fluid from the seminal vesicles also contains proteins, fructose (a simple sugar), and other substances that help nourish sperm.
Ejaculatory Ducts
The ejaculatory ducts form where the vas deferens join with the ducts of the seminal vesicles in the prostate gland. They connect the vas deferens with the urethra. The ejaculatory ducts carry sperm from the vas deferens, as well as secretions from the seminal vesicles and the prostate gland that together form semen. The substances secreted into semen by the glands as it passes through the ejaculatory ducts control its pH and provide nutrients to sperm, among other functions. The fluid itself provides sperm with a medium in which to “swim.”
Prostate Gland
The prostate gland is located just below the seminal vesicles. It is a walnut-sized organ that surrounds the urethra and its junction with the two ejaculatory ducts. The function of the prostate gland is to secrete a slightly alkaline fluid that constitutes close to 30 percent of the total volume of semen. The prostate fluid contains small quantities of proteins, such as enzymes. In addition, it has a very high concentration of zinc, which is an important nutrient for maintaining sperm quality and motility.
Bulbourethral Glands
Also called Cowper’s glands, the two bulbourethral glands are each about the size of a pea and located just below the prostate gland. The bulbourethral glands secrete a clear, alkaline fluid that is rich in proteins. Each of the glands has a short duct that carries the secretions into the urethra, where they make up a tiny percentage of the total volume of semen. The function of the bulbourethral secretions is to help lubricate the urethra and neutralize any urine (which is acidic) that may remain in the urethra.
The penis is the external male organ that has the reproductive function of delivering sperm to the female reproductive tract. This function is called intromission. The penis also serves as the organ that excretes urine.
Structure of the Penis
The structure of the penis and its location relative to other reproductive organs are shown in Figure \(\PageIndex{4}\). The part of the penis that is located inside the body and out of sight is called the root of the penis. The shaft of the penis is the part of the penis that is outside the body. The enlarged, bulbous end of the shaft is called the glans penis.
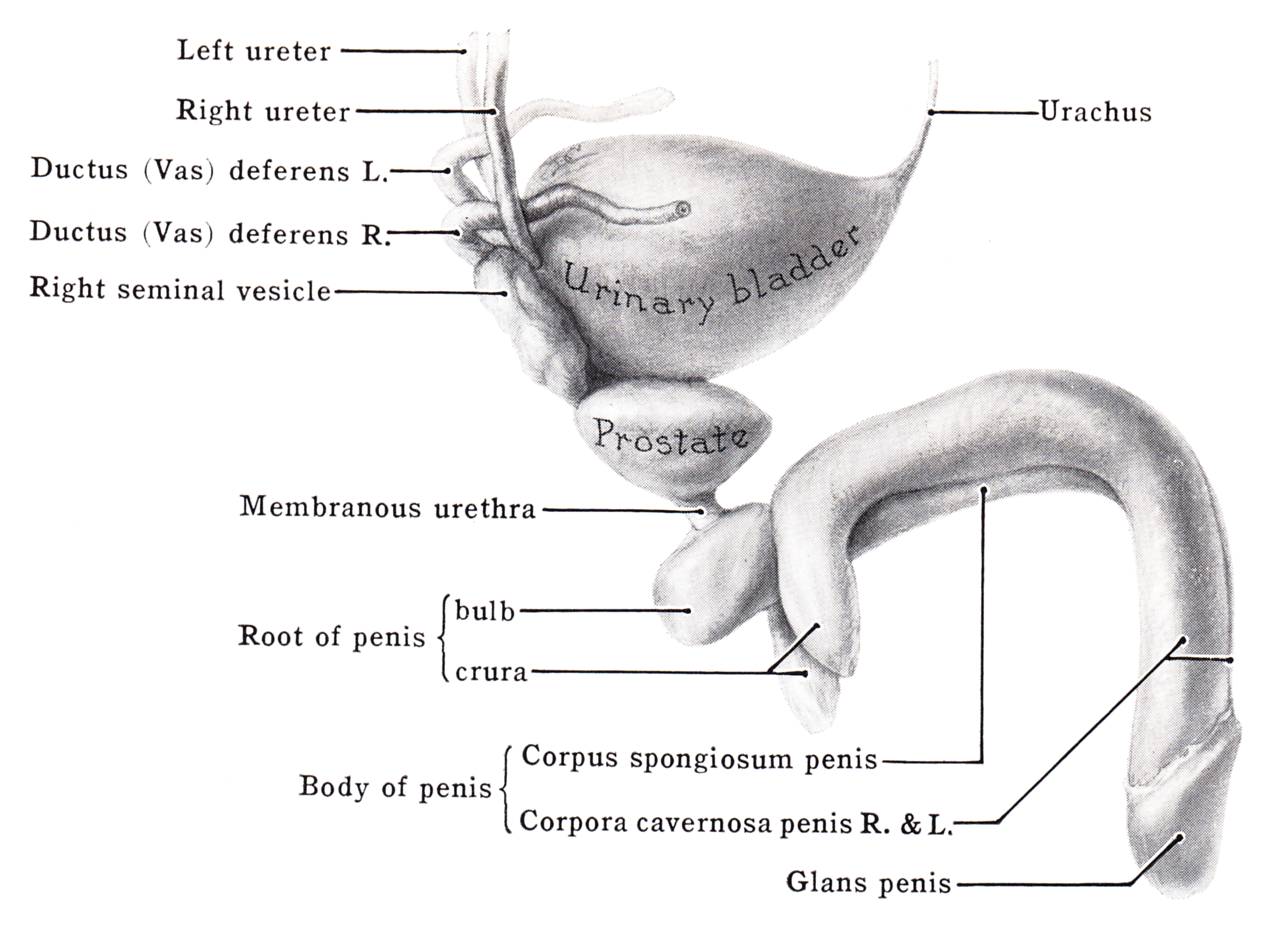
The urethra passes through the penis to carry urine from the bladder — or semen from the ejaculatory ducts — through the penis and out of the body. After leaving the urinary bladder, the urethra passes through the prostate gland, where the urethra is joined by the ejaculatory ducts. From there, the urethra passes through the penis to its external opening at the tip of the glans penis. Called the external urethral orifice, this opening provides a way for urine or semen to leave the body.
Tissues of the Penis
The penis is covered with skin (epithelium) that is unattached and free to move over the body of the penis. In an uncircumcised male, the glans penis is also mainly covered by epithelium, which (in this location) is called the foreskin, and below which is a layer of the mucous membrane. The foreskin is attached to the penis at an area on the underside of the penis called the frenulum.
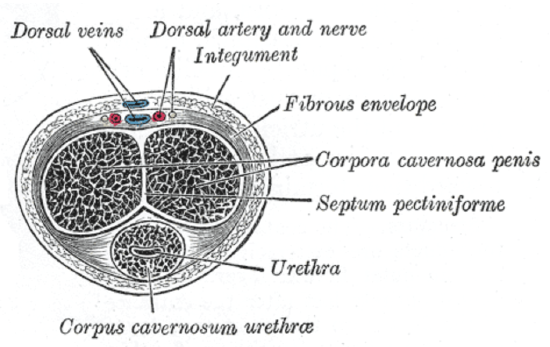
As shown in Figure \(\PageIndex{5}\), the interior of the penis consists of three columns of spongy tissue that can fill with blood and swell in size, allowing the penis to become erect. This spongy tissue is called corpus cavernosum (plural, corpora cavernosa). Two columns of this tissue run side by side along the top of the shaft, and one column runs along the bottom of the shaft. The urethra runs through this bottom column of spongy tissue, which is sometimes called corpus spongiosum. The glans penis also consists mostly of spongy erectile tissue. Veins and arteries run along the top of the penis, allowing blood circulation through the spongy tissues.
Feature: Human Biology in the News
Lung, heart, kidney, and other organ transplants have become relatively commonplace, so when they occur, they are unlikely to make the news. However, when the nation’s first penis transplant took place, it was considered very newsworthy.
In 2016, Massachusetts General Hospital in Boston announced that a team of its surgeons had performed the first penis transplant in the United States. The patient who received the donated penis was a 64-year-old cancer patient. During the 15-hour procedure, the intricate network of nerves and blood vessels of the donor penis were connected with those of the penis recipient. The surgery went well, but doctors reported it would be a few weeks until they would know if normal urination would be possible, and even longer before they would know if sexual functioning would be possible. At the time that news of the surgery was reported in the media, the patient had not shown any signs of rejecting the donated organ. The surgeons also reported they were hopeful that such transplants would become relatively common, and that patient populations would expand to include wounded warriors and transgender males seeking to transition.
The 2016 Massachusetts operation was not the first penis transplant ever undertaken. The world’s first successful penis transplant was actually performed in 2014 in Cape Town, South Africa. A young man who had lost his penis from complications of a botched circumcision at age 18 was given a donor penis three years later. That surgery lasted nine hours and was highly successful. The young man made a full recovery and regained both urinary and sexual functions in the transplanted organ.
In 2005, a man in China also received a donated penis in a technically successful operation. However, the patient asked doctors to reverse the procedure just two weeks later, because of psychological problems associated with the transplanted organ for both himself and his wife.
- What are the testes? Where are they located?
- Describe the structure of a testis.
- Identify the epididymis and its functions.
- What are the vas deferens? What do they do?
- Where are the seminal vesicles located? What is their reproductive role?
- Which parts of the male reproductive system are connected by the ejaculatory ducts? What fluids enter and leave the ejaculatory ducts?
- Identify the location of the prostate gland relative to other male reproductive organs. What is the prostate’s function?
- Where are the bulbourethral glands? What is their function?
- Relate the structure of the penis to its two basic functions.
- Sperm are produced here.
- Sperm mature here.
- Sperm are transported through the penis in this structure.
- This is a gland that produces fluid that is a major component of semen.
- A vasectomy is a form of birth control for men that is performed by surgically cutting or blocking the vas deferens so that sperm cannot be ejaculated out of the body. Do you think men who have a vasectomy emit semen when they ejaculate? Why or why not?
- seminal vesicles
- glans penis
Explore More
Morning erections are part of the normal sleep cycle in men. Learn more here:
Attributions
- Lamb Fries by Paul Lowry, CC BY 2.0 via Wikimedia Commons
- Testicle by (public domain; National Cancer Institute via Wikimedia.org )
- Male Reproductive Anatomy by OpenStax College licensed CC BY 3.0
- Anatomical Illustration by Grant, John Charles Boileau licensed public domain, via Wikimedia Commons
- Cross-section of the penis , by Gray's Anatomy, licensed public domain, via Wikimedia Commons
- Text adapted from Human Biology by CK-12 licensed CC BY-NC 3.0
Duct System
Sperm cells pass through a series of ducts to reach the outside of the body. After they leave the testes, the sperm passes through the epididymis , ductus deferens , ejaculatory duct , and urethra .
Sperm leave the testes through a series of efferent ducts that enter the epididymis. Each epididymis is a long (about 6 meters) tube that is tightly coiled to form a comma-shaped organ located along the superior and posterior margins of the testes. When the sperm leave the testes, they are immature and incapable of fertilizing ova . They complete their maturation process and become fertile as they move through the epididymis. Mature sperm are stored in the lower portion, or tail, of the epididymis.
Ductus Deferens
The ductus deferens, also called vas deferens , is a fibromuscular tube that is continuous ( or contiguous ) with the epididymis. It begins at the bottom (tail) of the epididymis then turns sharply upward along the posterior margin of the testes. The ductus deferens enters the abdominopelvic cavity through the inguinal canal and passes along the lateral pelvic wall . It crosses over the ureter and posterior portion of the urinary bladder , and then descends along the posterior wall of the bladder toward the prostate gland . Just before it reaches the prostate gland, each ductus deferens enlarges to form an ampulla. Sperm are stored in the proximal portion of the ductus deferens, near the epididymis, and peristaltic movements propel the sperm through the tube.
The proximal portion of the ductus deferens is a component of the spermatic cord , which contains vascular and neural structures that supply the testes. The spermatic cord contains the ductus deferens, testicular artery and veins , lymph vessels, testicular nerve , cremaster muscle that elevates the testes for warmth and at times of sexual stimulation, and a connective tissue covering.
Ejaculatory Duct
Each ductus deferens, at the ampulla , joins the duct from the adjacent seminal vesicle (one of the accessory glands) to form a short ejaculatory duct. Each ejaculatory duct passes through the prostate gland and empties into the urethra.
The urethra extends from the urinary bladder to the external urethral orifice at the tip of the penis . It is a passageway for sperm and fluids from the reproductive system and urine from the urinary system . While reproductive fluids are passing through the urethra, sphincters contract tightly to keep urine from entering the urethra.
The male urethra is divided into three regions. The prostatic urethra is the proximal portion that passes through the prostate gland. It receives the ejaculatory duct, which contains sperm and secretions from the seminal vesicles , and numerous ducts from the prostate glands. The next portion, the membranous urethra , is a short region that passes through the pelvic floor . The longest portion is the penile urethra (also called spongy urethra or cavernous urethra), which extends the length of the penis and opens to the outside at the external urethral orifice. The ducts from the bulbourethral glands open into the penile urethra.
Chapter 11: The Reproductive System
The male reproductive system, learning objectives.
By the end of this section, you will be able to:
- Describe the structure and basic functions of the male gonads.
- Describe the function of the seminiferous tubules and interstitial cells.
- Describe the characteristic and advantage of the vascular supply to the testis.
- Describe the structure and function of the epididymides.
- Describe the structure, and function of the ductus deferentia.
- Describe the structure, and function of the seminal vesicles.
- Describe the structure, and function of the prostate gland.
- Describe the function of the bulbourethral glands.
- Identify the approximate percentage of semen contributed by the testes, seminal vesicles, and prostate gland.
- Describe the physiological mechanism of erection.
- Describe the physiological mechanism of ejaculation.
- Discuss the process of spermatogonium formation.
- Describe the process of meiosis in males.
- Explain the process of spermiogenesis and describe the morphological changes that occur as a spermatid becomes a spermatozoon.
- Describe the role that sustentacular cells play in spermatogenesis.
- Describe the braintesticular axis. Include the following terms in your discussion: hypothalamus, gonadotropin releasing hormone, follicle stimulating hormone, luteinizing hormone, anterior pituitary gland, sustentacular cells, interstitial cells, and testosterone.
- Describe the mechanism regulating sperm and testosterone production.
- Describe the somatic effects of testosterone and its influence on male secondary sexual characteristics.
Unique for its role in human reproduction, a gamete is a specialized sex cell carrying 23 chromosomes—one half the number in body cells. At fertilization, the chromosomes in one male gamete, called a sperm (or spermatozoon), combine with the chromosomes in one female gamete, called an oocyte. The function of the male reproductive system is to produce sperm and transfer them to the female reproductive tract. The paired testes are a crucial component in this process, as they produce both sperm and androgens, the hormones that support male reproductive physiology. In humans, the most important male androgen is testosterone. Several accessory organs and ducts aid the process of sperm maturation and transport the sperm and other seminal components to the penis, which delivers sperm to the female reproductive tract. In this section, we examine each of these different structures, and discuss the process of sperm production and transport.

Figure 1. Click for a larger image. The structures of the male reproductive system include the testes, the epididymides, the penis, and the ducts and glands that produce and carry semen. Sperm exit the scrotum through the ductus deferens, which is bundled in the spermatic cord. The seminal vesicles and prostate gland add fluids to the sperm to create semen.
The testes are located in a skin-covered, highly pigmented, muscular sack called the scrotum that extends from the body behind the penis. This location is important in sperm production, which occurs within the testes, and proceeds more efficiently when the testes are kept 2 to 4°C below core body temperature.
The dartos muscle makes up the subcutaneous muscle layer of the scrotum. It continues internally to make up the scrotal septum, a wall that divides the scrotum into two compartments, each housing one testis. Descending from the internal oblique muscle of the abdominal wall are the two cremaster muscles, which cover each testis like a muscular net. By contracting simultaneously, the dartos and cremaster muscles can elevate the testes in cold weather (or water), moving the testes closer to the body and decreasing the surface area of the scrotum to retain heat. Alternatively, as the environmental temperature increases, the scrotum relaxes, moving the testes farther from the body core and increasing scrotal surface area, which promotes heat loss. Externally, the scrotum has a raised medial thickening on the surface called the raphe.

Figure 2. This anterior view shows the structures of the scrotum and testes.
The testes (singular = testis) are the male gonads —that is, the male reproductive organs. They produce both sperm and androgens, such as testosterone, and are active throughout the reproductive lifespan of the male.

Figure 3. This sagittal view shows the seminiferous tubules, the site of sperm production. Formed sperm are transferred to the epididymis, where they mature. They leave the epididymis during an ejaculation via the ductus deferens.
Paired ovals, the testes are each approximately 4 to 5 cm in length and are housed within the scrotum. They are surrounded by two distinct layers of protective connective tissue. The outer tunica vaginalis is a serous membrane that has both a parietal and a thin visceral layer. Beneath the tunica vaginalis is the tunica albuginea, a tough, white, dense connective tissue layer covering the testis itself. Not only does the tunica albuginea cover the outside of the testis, it also invaginates to form septa that divide the testis into 300 to 400 structures called lobules. Within the lobules, sperm develop in structures called seminiferous tubules. During the seventh month of the developmental period of a male fetus, each testis moves through the abdominal musculature to descend into the scrotal cavity. This is called the “descent of the testis.” Cryptorchidism is the clinical term used when one or both of the testes fail to descend into the scrotum prior to birth.
The tightly coiled seminiferous tubules form the bulk of each testis. They are composed of developing sperm cells surrounding a lumen, the hollow center of the tubule, where formed sperm are released into the duct system of the testis. Specifically, from the lumens of the seminiferous tubules, sperm move into the straight tubules (or tubuli recti), and from there into a fine meshwork of tubules called the rete testes. Sperm leave the rete testes, and the testis itself, through the 15 to 20 efferent ductules that cross the tunica albuginea.
Spermatogenesis
Spermatogenesis is the term for the development of sperm. This process occurs in the seminiferous tubules that form the bulk of each testis. The process begins at puberty, after which time sperm are produced constantly throughout a man’s life. One production cycle, from spermatogonia through formed sperm, takes approximately 64 days. A new cycle starts approximately every 16 days, although this timing is not synchronous across the seminiferous tubules. Sperm counts—the total number of sperm a man produces—slowly decline after age 35, and some studies suggest that smoking can lower sperm counts irrespective of age.
The process of spermatogenesis begins with mitosis of the diploid spermatogonia. Because these cells are diploid (2 n ), they each have a complete copy of the father’s genetic material, or 46 chromosomes. However, mature gametes are haploid (1 n ), containing 23 chromosomes—meaning that daughter cells of spermatogonia must undergo a second cellular division through the process of meiosis.

Figure 4. (a) Mitosis of a spermatogonial stem cell involves a single cell division that results in two identical, diploid daughter cells (spermatogonia to primary spermatocyte). Meiosis has two rounds of cell division: primary spermatocyte to secondary spermatocyte, and then secondary spermatocyte to spermatid. This produces four haploid daughter cells (spermatids). (b) In this electron micrograph of a cross-section of a seminiferous tubule from a rat, the lumen is the light-shaded area in the center of the image. The location of the primary spermatocytes is near the basement membrane, and the early spermatids are approaching the lumen (tissue source: rat). EM × 900. (Micrograph provided by the Regents of University of Michigan Medical School © 2012)
Two identical diploid cells result from spermatogonia mitosis. One of these cells remains a spermatogonium, and the other becomes a primary spermatocyte , the next stage in the process of spermatogenesis. As in mitosis, DNA is replicated in a primary spermatocyte, and the cell undergoes cell division to produce two cells with identical chromosomes. Each of these is a secondary spermatocyte. Now a second round of cell division occurs in both of the secondary spermatocytes, separating the chromosome pairs. This second meiotic division results in a total of four cells with only half of the number of chromosomes. Each of these new cells is a spermatid . Although haploid, early spermatids look very similar to cells in the earlier stages of spermatogenesis, with a round shape, central nucleus, and large amount of cytoplasm. A process called spermiogenesis transforms these early spermatids, reducing the cytoplasm, and beginning the formation of the parts of a true sperm. The fifth stage of germ cell formation—spermatozoa, or formed sperm—is the end result of this process, which occurs in the portion of the tubule nearest the lumen. Eventually, the sperm are released into the lumen and are moved along a series of ducts in the testis toward a structure called the epididymis for the next step of sperm maturation.
Structure of Formed Sperm
Sperm are smaller than most cells in the body; in fact, the volume of a sperm cell is 85,000 times less than that of the female gamete. Approximately 100 to 300 million sperm are produced each day, whereas women typically ovulate only one oocyte per month as is true for most cells in the body, the structure of sperm cells speaks to their function. Sperm have a distinctive head, mid-piece, and tail region. The head of the sperm contains the extremely compact haploid nucleus with very little cytoplasm. These qualities contribute to the overall small size of the sperm (the head is only 5 μ m long). A structure called the acrosome covers most of the head of the sperm cell as a “cap” that is filled with lysosomal enzymes important for preparing sperm to participate in fertilization. Tightly packed mitochondria fill the mid-piece of the sperm. ATP produced by these mitochondria will power the flagellum, which extends from the neck and the mid-piece through the tail of the sperm, enabling it to move the entire sperm cell. The central strand of the flagellum, the axial filament, is formed from one centriole inside the maturing sperm cell during the final stages of spermatogenesis.

Figure 5. Sperm cells are divided into a head, containing DNA; a mid-piece, containing mitochondria; and a tail, providing motility. The acrosome is oval and somewhat flattened.
Sperm Transport
To fertilize an egg, sperm must be moved from the seminiferous tubules in the testes, through the epididymis, and—later during ejaculation—along the length of the penis and out into the female reproductive tract.
From the lumen of the seminiferous tubules, the immotile sperm are surrounded by testicular fluid and moved to the epididymis (plural = epididymides), a coiled tube attached to the testis where newly formed sperm continue to mature. Though the epididymis does not take up much room in its tightly coiled state, it would be approximately 6 m (20 feet) long if straightened. It takes an average of 12 days for sperm to move through the coils of the epididymis, with the shortest recorded transit time in humans being one day. Sperm enter the head of the epididymis and are moved along predominantly by the contraction of smooth muscles lining the epididymal tubes. As they are moved along the length of the epididymis, the sperm further mature and acquire the ability to move under their own power. Once inside the female reproductive tract, they will use this ability to move independently toward the unfertilized egg. The more mature sperm are then stored in the tail of the epididymis (the final section) until ejaculation occurs.
Duct System
During ejaculation, sperm exit the tail of the epididymis and are pushed by smooth muscle contraction to the ductus deferens (also called the vas deferens). The ductus deferens is a thick, muscular tube that is bundled together inside the scrotum with connective tissue, blood vessels, and nerves into a structure called the spermatic cord . Because the ductus deferens is physically accessible within the scrotum, surgical sterilization to interrupt sperm delivery can be performed by cutting and sealing a small section of the ductus (vas) deferens. This procedure is called a vasectomy, and it is an effective form of male birth control. Although it may be possible to reverse a vasectomy, clinicians consider the procedure permanent, and advise men to undergo it only if they are certain they no longer wish to father children.
Practice Question
Watch this video to learn about a vasectomy. As described in this video, a vasectomy is a procedure in which a small section of the ductus (vas) deferens is removed from the scrotum. This interrupts the path taken by sperm through the ductus deferens. If sperm do not exit through the vas, either because the man has had a vasectomy or has not ejaculated, in what region of the testis do they remain?
From each epididymis, each ductus deferens extends superiorly into the abdominal cavity through the inguinal canal in the abdominal wall. From here, the ductus deferens continues posteriorly to the pelvic cavity, ending posterior to the bladder where it dilates in a region called the ampulla (meaning “flask”).
Sperm make up only 5 percent of the final volume of semen , the thick, milky fluid that the male ejaculates. The bulk of semen is produced by three critical accessory glands of the male reproductive system: the seminal vesicles, the prostate, and the bulbourethral glands.
Seminal Vesicles
As sperm pass through the ampulla of the ductus deferens at ejaculation, they mix with fluid from the associated seminal vesicle . The paired seminal vesicles are glands that contribute approximately 60 percent of the semen volume. Seminal vesicle fluid contains large amounts of fructose, which is used by the sperm mitochondria to generate ATP to allow movement through the female reproductive tract.
The fluid, now containing both sperm and seminal vesicle secretions, next moves into the associated ejaculatory duct , a short structure formed from the ampulla of the ductus deferens and the duct of the seminal vesicle. The paired ejaculatory ducts transport the seminal fluid into the next structure, the prostate gland.
Prostate Gland
As shown in Figure 1, the centrally located prostate gland sits anterior to the rectum at the base of the bladder surrounding the prostatic urethra (the portion of the urethra that runs within the prostate). About the size of a walnut, the prostate is formed of both muscular and glandular tissues. It excretes an alkaline, milky fluid to the passing seminal fluid—now called semen—that is critical to first coagulate and then decoagulate the semen following ejaculation. The temporary thickening of semen helps retain it within the female reproductive tract, providing time for sperm to utilize the fructose provided by seminal vesicle secretions. When the semen regains its fluid state, sperm can then pass farther into the female reproductive tract.
The prostate normally doubles in size during puberty. At approximately age 25, it gradually begins to enlarge again. This enlargement does not usually cause problems; however, abnormal growth of the prostate, or benign prostatic hyperplasia (BPH), can cause constriction of the urethra as it passes through the middle of the prostate gland, leading to a number of lower urinary tract symptoms, such as a frequent and intense urge to urinate, a weak stream, and a sensation that the bladder has not emptied completely. By age 60, approximately 40 percent of men have some degree of BPH. By age 80, the number of affected individuals has jumped to as many as 80 percent. Treatments for BPH attempt to relieve the pressure on the urethra so that urine can flow more normally. Mild to moderate symptoms are treated with medication, whereas severe enlargement of the prostate is treated by surgery in which a portion of the prostate tissue is removed.
Another common disorder involving the prostate is prostate cancer. According to the Centers for Disease Control and Prevention (CDC), prostate cancer is the second most common cancer in men. However, some forms of prostate cancer grow very slowly and thus may not ever require treatment. Aggressive forms of prostate cancer, in contrast, involve metastasis to vulnerable organs like the lungs and brain. There is no link between BPH and prostate cancer, but the symptoms are similar. Prostate cancer is detected by a medical history, a blood test, and a rectal exam that allows physicians to palpate the prostate and check for unusual masses. If a mass is detected, the cancer diagnosis is confirmed by biopsy of the cells.
Bulbourethral Glands
The final addition to semen is made by two bulbourethral glands (or Cowper’s glands) that release a thick, salty fluid that lubricates the end of the urethra and the vagina, and helps to clean urine residues from the penile urethra. The fluid from these accessory glands is released after the male becomes sexually aroused, and shortly before the release of the semen. It is therefore sometimes called pre-ejaculate. It is important to note that, in addition to the lubricating proteins, it is possible for bulbourethral fluid to pick up sperm already present in the urethra, and therefore it may be able to cause pregnancy.
Practice Question
Watch this video to explore the structures of the male reproductive system and the path of sperm , which starts in the testes and ends as the sperm leave the penis through the urethra. Where are sperm deposited after they leave the ejaculatory duct?
The penis is the male organ of copulation (sexual intercourse). It is flaccid for non-sexual actions, such as urination, and turgid and rod-like with sexual arousal. When erect, the stiffness of the organ allows it to penetrate into the vagina and deposit semen into the female reproductive tract.

Figure 6. Three columns of erectile tissue make up most of the volume of the penis.
The shaft of the penis surrounds the urethra. The shaft is composed of three column-like chambers of erectile tissue that span the length of the shaft. Each of the two larger lateral chambers is called a corpus cavernosum (plural = corpora cavernosa). Together, these make up the bulk of the penis. The corpus spongiosum , which can be felt as a raised ridge on the erect penis, is a smaller chamber that surrounds the spongy, or penile, urethra. The end of the penis, called the glans penis , has a high concentration of nerve endings, resulting in very sensitive skin that influences the likelihood of ejaculation. The skin from the shaft extends down over the glans and forms a collar called the prepuce (or foreskin). The foreskin also contains a dense concentration of nerve endings, and both lubricate and protect the sensitive skin of the glans penis. A surgical procedure called circumcision, often performed for religious or social reasons, removes the prepuce, typically within days of birth.
Both sexual arousal and REM sleep (during which dreaming occurs) can induce an erection. Penile erections are the result of vasocongestion, or engorgement of the tissues because of more arterial blood flowing into the penis than is leaving in the veins. During sexual arousal, nitric oxide (NO) is released from nerve endings near blood vessels within the corpora cavernosa and spongiosum. Release of NO activates a signaling pathway that results in relaxation of the smooth muscles that surround the penile arteries, causing them to dilate. This dilation increases the amount of blood that can enter the penis and induces the endothelial cells in the penile arterial walls to also secrete NO and perpetuate the vasodilation. The rapid increase in blood volume fills the erectile chambers, and the increased pressure of the filled chambers compresses the thin-walled penile venules, preventing venous drainage of the penis. The result of this increased blood flow to the penis and reduced blood return from the penis is erection. Depending on the flaccid dimensions of a penis, it can increase in size slightly or greatly during erection, with the average length of an erect penis measuring approximately 15 cm.
Disorders of the Male Reproductive System: Erectile dysfunction (ED)
Erectile dysfunction (ED) is a condition in which a man has difficulty either initiating or maintaining an erection. The combined prevalence of minimal, moderate, and complete ED is approximately 40 percent in men at age 40, and reaches nearly 70 percent by 70 years of age. In addition to aging, ED is associated with diabetes, vascular disease, psychiatric disorders, prostate disorders, the use of some drugs such as certain antidepressants, and problems with the testes resulting in low testosterone concentrations. These physical and emotional conditions can lead to interruptions in the vasodilation pathway and result in an inability to achieve an erection.
Recall that the release of NO induces relaxation of the smooth muscles that surround the penile arteries, leading to the vasodilation necessary to achieve an erection. To reverse the process of vasodilation, an enzyme called phosphodiesterase (PDE) degrades a key component of the NO signaling pathway called cGMP. There are several different forms of this enzyme, and PDE type 5 is the type of PDE found in the tissues of the penis. Scientists discovered that inhibiting PDE5 increases blood flow, and allows vasodilation of the penis to occur.
PDEs and the vasodilation signaling pathway are found in the vasculature in other parts of the body. In the 1990s, clinical trials of a PDE5 inhibitor called sildenafil were initiated to treat hypertension and angina pectoris (chest pain caused by poor blood flow through the heart). The trial showed that the drug was not effective at treating heart conditions, but many men experienced erection and priapism (erection lasting longer than 4 hours). Because of this, a clinical trial was started to investigate the ability of sildenafil to promote erections in men suffering from ED. In 1998, the FDA approved the drug, marketed as Viagra ® . Since approval of the drug, sildenafil and similar PDE inhibitors now generate over a billion dollars a year in sales, and are reported to be effective in treating approximately 70 to 85 percent of cases of ED. Importantly, men with health problems—especially those with cardiac disease taking nitrates—should avoid Viagra or talk to their physician to find out if they are a candidate for the use of this drug, as deaths have been reported for at-risk users.
Testosterone
Testosterone, an androgen, is a steroid hormone produced by Leydig cells . The alternate term for Leydig cells, interstitial cells, reflects their location between the seminiferous tubules in the testes. In male embryos, testosterone is secreted by Leydig cells by the seventh week of development, with peak concentrations reached in the second trimester. This early release of testosterone results in the anatomical differentiation of the male sexual organs. In childhood, testosterone concentrations are low. They increase during puberty, activating characteristic physical changes and initiating spermatogenesis.
Functions of Testosterone
The continued presence of testosterone is necessary to keep the male reproductive system working properly, and Leydig cells produce approximately 6 to 7 mg of testosterone per day. Testicular steroidogenesis (the manufacture of androgens, including testosterone) results in testosterone concentrations that are 100 times higher in the testes than in the circulation. Maintaining these normal concentrations of testosterone promotes spermatogenesis, whereas low levels of testosterone can lead to infertility. In addition to intratesticular secretion, testosterone is also released into the systemic circulation and plays an important role in muscle development, bone growth, the development of secondary sex characteristics, and maintaining libido (sex drive) in both males and females. In females, the ovaries secrete small amounts of testosterone, although most is converted to estradiol. A small amount of testosterone is also secreted by the adrenal glands in both sexes.
Regulation of Testosterone
The regulation of testosterone concentrations throughout the body is critical for male reproductive function. The intricate interplay between the endocrine system and the reproductive system is shown in Figure 7.

Figure 7. The hypothalamus and pituitary gland regulate the production of testosterone and the cells that assist in spermatogenesis. GnRH activates the anterior pituitary to produce LH and FSH, which in turn stimulate Leydig cells and Sertoli cells, respectively. The system is a negative feedback loop because the end products of the pathway, testosterone and inhibin, interact with the activity of GnRH to inhibit their own production.
The regulation of Leydig cell production of testosterone begins outside of the testes. The hypothalamus and the pituitary gland in the brain integrate external and internal signals to control testosterone synthesis and secretion. The regulation begins in the hypothalamus. Pulsatile release of a hormone called gonadotropin-releasing hormone (GnRH) from the hypothalamus stimulates the endocrine release of hormones from the pituitary gland. Binding of GnRH to its receptors on the anterior pituitary gland stimulates release of the two gonadotropins: luteinizing hormone (LH) and follicle-stimulating hormone (FSH). These two hormones are critical for reproductive function in both men and women. In men, FSH binds predominantly to the Sertoli cells within the seminiferous tubules to promote spermatogenesis. FSH also stimulates the Sertoli cells to produce hormones called inhibins, which function to inhibit FSH release from the pituitary, thus reducing testosterone secretion. These polypeptide hormones correlate directly with Sertoli cell function and sperm number; inhibin B can be used as a marker of spermatogenic activity. In men, LH binds to receptors on Leydig cells in the testes and upregulates the production of testosterone.
A negative feedback loop predominantly controls the synthesis and secretion of both FSH and LH. Low blood concentrations of testosterone stimulate the hypothalamic release of GnRH. GnRH then stimulates the anterior pituitary to secrete LH into the bloodstream. In the testis, LH binds to LH receptors on Leydig cells and stimulates the release of testosterone. When concentrations of testosterone in the blood reach a critical threshold, testosterone itself will bind to androgen receptors on both the hypothalamus and the anterior pituitary, inhibiting the synthesis and secretion of GnRH and LH, respectively. When the blood concentrations of testosterone once again decline, testosterone no longer interacts with the receptors to the same degree and GnRH and LH are once again secreted, stimulating more testosterone production. This same process occurs with FSH and inhibin to control spermatogenesis.
Aging and the Male Reproductive System
Declines in Leydig cell activity can occur in men beginning at 40 to 50 years of age. The resulting reduction in circulating testosterone concentrations can lead to symptoms of andropause, also known as male menopause. While the reduction in sex steroids in men is akin to female menopause, there is no clear sign—such as a lack of a menstrual period—to denote the initiation of andropause. Instead, men report feelings of fatigue, reduced muscle mass, depression, anxiety, irritability, loss of libido, and insomnia. A reduction in spermatogenesis resulting in lowered fertility is also reported, and sexual dysfunction can also be associated with andropausal symptoms.
Whereas some researchers believe that certain aspects of andropause are difficult to tease apart from aging in general, testosterone replacement is sometimes prescribed to alleviate some symptoms. Recent studies have shown a benefit from androgen replacement therapy on the new onset of depression in elderly men; however, other studies caution against testosterone replacement for long-term treatment of andropause symptoms, showing that high doses can sharply increase the risk of both heart disease and prostate cancer.
Chapter Review
Gametes are the reproductive cells that combine to form offspring. Organs called gonads produce the gametes, along with the hormones that regulate human reproduction. The male gametes are called sperm. Spermatogenesis, the production of sperm, occurs within the seminiferous tubules that make up most of the testis. The scrotum is the muscular sac that holds the testes outside of the body cavity.
Spermatogenesis begins with mitotic division of spermatogonia (stem cells) to produce primary spermatocytes that undergo the two divisions of meiosis to become secondary spermatocytes, then the haploid spermatids. During spermiogenesis, spermatids are transformed into spermatozoa (formed sperm). Upon release from the seminiferous tubules, sperm are moved to the epididymis where they continue to mature. During ejaculation, sperm exit the epididymis through the ductus deferens, a duct in the spermatic cord that leaves the scrotum. The ampulla of the ductus deferens meets the seminal vesicle, a gland that contributes fructose and proteins, at the ejaculatory duct. The fluid continues through the prostatic urethra, where secretions from the prostate are added to form semen. These secretions help the sperm to travel through the urethra and into the female reproductive tract. Secretions from the bulbourethral glands protect sperm and cleanse and lubricate the penile (spongy) urethra.
The penis is the male organ of copulation. Columns of erectile tissue called the corpora cavernosa and corpus spongiosum fill with blood when sexual arousal activates vasodilatation in the blood vessels of the penis. Testosterone regulates and maintains the sex organs and sex drive, and induces the physical changes of puberty. Interplay between the testes and the endocrine system precisely control the production of testosterone with a negative feedback loop.
blood–testis barrier: tight junctions between Sertoli cells that prevent bloodborne pathogens from gaining access to later stages of spermatogenesis and prevent the potential for an autoimmune reaction to haploid sperm
bulbourethral glands: (also, Cowper’s glands) glands that secrete a lubricating mucus that cleans and lubricates the urethra prior to and during ejaculation
corpus cavernosum: either of two columns of erectile tissue in the penis that fill with blood during an erection
corpus spongiosum: (plural = corpora cavernosa) column of erectile tissue in the penis that fills with blood during an erection and surrounds the penile urethra on the ventral portion of the penis
ductus deferens: (also, vas deferens) duct that transports sperm from the epididymis through the spermatic cord and into the ejaculatory duct; also referred as the vas deferens
ejaculatory duct: duct that connects the ampulla of the ductus deferens with the duct of the seminal vesicle at the prostatic urethra
epididymis: (plural = epididymides) coiled tubular structure in which sperm start to mature and are stored until ejaculation
gamete: haploid reproductive cell that contributes genetic material to form an offspring
glans penis: bulbous end of the penis that contains a large number of nerve endings
gonadotropin-releasing hormone (GnRH): hormone released by the hypothalamus that regulates the production of follicle-stimulating hormone and luteinizing hormone from the pituitary gland
gonads: reproductive organs (testes in men and ovaries in women) that produce gametes and reproductive hormones
inguinal canal: opening in abdominal wall that connects the testes to the abdominal cavity
Leydig cells: cells between the seminiferous tubules of the testes that produce testosterone; a type of interstitial cell
penis: male organ of copulation
prepuce: (also, foreskin) flap of skin that forms a collar around, and thus protects and lubricates, the glans penis; also referred as the foreskin
prostate gland: doughnut-shaped gland at the base of the bladder surrounding the urethra and contributing fluid to semen during ejaculation
scrotum: external pouch of skin and muscle that houses the testes
semen: ejaculatory fluid composed of sperm and secretions from the seminal vesicles, prostate, and bulbourethral glands
seminal vesicle: gland that produces seminal fluid, which contributes to semen
seminiferous tubules: tube structures within the testes where spermatogenesis occurs
Sertoli cells: cells that support germ cells through the process of spermatogenesis; a type of sustentacular cell
sperm: (also, spermatozoon) male gamete
spermatic cord: bundle of nerves and blood vessels that supplies the testes; contains ductus deferens
spermatid: immature sperm cells produced by meiosis II of secondary spermatocytes
spermatocyte: cell that results from the division of spermatogonium and undergoes meiosis I and meiosis II to form spermatids
spermatogenesis: formation of new sperm, occurs in the seminiferous tubules of the testes
spermatogonia: (singular = spermatogonium) diploid precursor cells that become sperm
spermiogenesis: transformation of spermatids to spermatozoa during spermatogenesis
testes: (singular = testis) male gonads

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

- Health Topics
- Drugs & Supplements
- Medical Tests
- Medical Encyclopedia
- About MedlinePlus
- Customer Support
Pathway of sperm
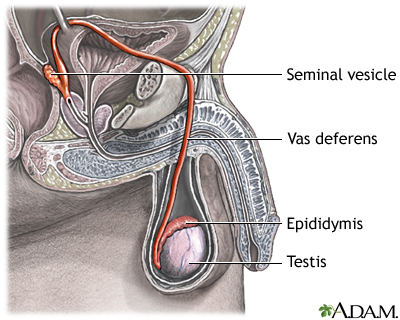
The testes are where sperm are manufactured in the scrotum. The epididymis is a tortuously coiled structure topping the testis, and it receives immature sperm from the testis and stores it for several days. When ejaculation occurs, sperm is forcefully expelled from the tail of the epididymis into the deferent duct. Sperm then travels through the deferent duct through up the spermatic cord into the pelvic cavity, over the ureter to the prostate behind the bladder. Here, the vas deferens joins with the seminal vesicle to form the ejaculatory duct, which passes through the prostate and empties into the urethra. When ejaculation occurs, rhythmic muscle movements propel the sperm forward.
Review Date 7/4/2022
Updated by: Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

23.2: Anatomy and Physiology of the Male Reproductive System
- Last updated
- Save as PDF
- Page ID 61638

Learning Objectives
- Describe the structure and function of the organs of the male reproductive system
- Describe the structure and function of the sperm cell
- Explain the events during spermatogenesis that produce haploid sperm from diploid cells
- Identify the importance of testosterone in male reproductive function
Unique for its role in human reproduction, a gamete is a specialized sex cell carrying 23 chromosomes—one half the number in body cells. At fertilization, the chromosomes in one male gamete, called a sperm (or spermatozoon), combine with the chromosomes in one female gamete, called an oocyte. The function of the male reproductive system (Figure \(\PageIndex{1}\)) is to produce sperm and transfer them to the female reproductive tract. The paired testes are a crucial component in this process, as they produce both sperm and androgens, the hormones that support male reproductive physiology. In humans, the most important male androgen is testosterone. Several accessory organs and ducts aid the process of sperm maturation and transport the sperm and other seminal components to the penis, which delivers sperm to the female reproductive tract. In this section, we examine each of these different structures, and discuss the process of sperm production and transport.

The testes are located in a skin-covered, highly pigmented, muscular sack called the scrotum that extends from the body behind the penis (see Figure \(\PageIndex{1}\)). This location is important in sperm production, which occurs within the testes, and proceeds more efficiently when the testes are kept 2 to 4°C below core body temperature.
The dartos muscle makes up the subcutaneous muscle layer of the scrotum (Figure \(\PageIndex{2}\)). It continues internally to make up the scrotal septum, a wall that divides the scrotum into two compartments, each housing one testis. Descending from the internal oblique muscle of the abdominal wall are the two cremaster muscles, which cover each testis like a muscular net. By contracting simultaneously, the dartos and cremaster muscles can elevate the testes in cold weather (or water), moving the testes closer to the body and decreasing the surface area of the scrotum to retain heat. Alternatively, as the environmental temperature increases, the scrotum relaxes, moving the testes farther from the body core and increasing scrotal surface area, which promotes heat loss. Externally, the scrotum has a raised medial thickening on the surface called the raphae.
The testes (singular = testis) are the male gonads —that is, the male reproductive organs. They produce both sperm and androgens, such as testosterone, and are active throughout the reproductive lifespan of the male.
Paired ovals, the testes are each approximately 4 to 5 cm in length and are housed within the scrotum (see Figure \(\PageIndex{2}\)). They are surrounded by two distinct layers of protective connective tissue (Figure \(\PageIndex{3}\)). The outer tunica vaginalis is a serous membrane that has both a parietal and a thin visceral layer. Beneath the tunica vaginalis is the tunica albuginea, a tough, white, dense connective tissue layer covering the testis itself. Not only does the tunica albuginea cover the outside of the testis, it also invaginates to form septa that divide the testis into 300 to 400 structures called lobules. Within the lobules, sperm develop in structures called seminiferous tubules. During the seventh month of the developmental period of a male fetus, each testis moves through the abdominal musculature to descend into the scrotal cavity. This is called the “descent of the testis.” Cryptorchidism is the clinical term used when one or both of the testes fail to descend into the scrotum prior to birth.
The tightly coiled seminiferous tubules form the bulk of each testis. They are composed of developing sperm cells surrounding a lumen, the hollow center of the tubule, where formed sperm are released into the duct system of the testis. Specifically, from the lumens of the seminiferous tubules, sperm move into the straight tubules (or tubuli recti), and from there into a fine meshwork of tubules called the rete testes. Sperm leave the rete testes, and the testis itself, through the 15 to 20 efferent ductules that cross the tunica albuginea.
Inside the seminiferous tubules are six different cell types. These include supporting cells called sustentacular cells, as well as five types of developing sperm cells called germ cells. Germ cell development progresses from the basement membrane—at the perimeter of the tubule—toward the lumen. Let’s look more closely at these cell types.
Sertoli Cells
Surrounding all stages of the developing sperm cells are elongate, branching Sertoli cells . Sertoli cells are a type of supporting cell called a sustentacular cell, or sustenocyte, that are typically found in epithelial tissue. Sertoli cells secrete signaling molecules that promote sperm production and can control whether germ cells live or die. They extend physically around the germ cells from the peripheral basement membrane of the seminiferous tubules to the lumen. Tight junctions between these sustentacular cells create the blood–testis barrier , which keeps bloodborne substances from reaching the germ cells and, at the same time, keeps surface antigens on developing germ cells from escaping into the bloodstream and prompting an autoimmune response.
The least mature cells, the spermatogonia (singular = spermatogonium), line the basement membrane inside the tubule. Spermatogonia are the stem cells of the testis, which means that they are still able to differentiate into a variety of different cell types throughout adulthood. Spermatogonia divide to produce primary and secondary spermatocytes, then spermatids, which finally produce formed sperm. The process that begins with spermatogonia and concludes with the production of sperm is called spermatogenesis .
Spermatogenesis
As just noted, spermatogenesis occurs in the seminiferous tubules that form the bulk of each testis (see Figure \(\PageIndex{3}\)). The process begins at puberty, after which time sperm are produced constantly throughout a man’s life. One production cycle, from spermatogonia through formed sperm, takes approximately 64 days. A new cycle starts approximately every 16 days, although this timing is not synchronous across the seminiferous tubules. Sperm counts—the total number of sperm a man produces—slowly decline after age 35, and some studies suggest that smoking can lower sperm counts irrespective of age.
The process of spermatogenesis begins with mitosis of the diploid spermatogonia (Figure \(\PageIndex{4}\)). Because these cells are diploid (2 n ), they each have a complete copy of the father’s genetic material, or 46 chromosomes. However, mature gametes are haploid (1 n ), containing 23 chromosomes—meaning that daughter cells of spermatogonia must undergo a second cellular division through the process of meiosis.

Two identical diploid cells result from spermatogonia mitosis. One of these cells remains a spermatogonium, and the other becomes a primary spermatocyte , the next stage in the process of spermatogenesis. As in mitosis, DNA is replicated in a primary spermatocyte, and the cell undergoes cell division to produce two cells with identical chromosomes. Each of these is a secondary spermatocyte. Now a second round of cell division occurs in both of the secondary spermatocytes, separating the chromosome pairs. This second meiotic division results in a total of four cells with only half of the number of chromosomes. Each of these new cells is a spermatid . Although haploid, early spermatids look very similar to cells in the earlier stages of spermatogenesis, with a round shape, central nucleus, and large amount of cytoplasm. A process called spermiogenesis transforms these early spermatids, reducing the cytoplasm, and beginning the formation of the parts of a true sperm. The fifth stage of germ cell formation—spermatozoa, or formed sperm—is the end result of this process, which occurs in the portion of the tubule nearest the lumen. Eventually, the sperm are released into the lumen and are moved along a series of ducts in the testis toward a structure called the epididymis for the next step of sperm maturation.
Structure of Formed Sperm
Sperm are smaller than most cells in the body; in fact, the volume of a sperm cell is 85,000 times less than that of the female gamete. Approximately 100 to 300 million sperm are produced each day, whereas women typically ovulate only one oocyte per month as is true for most cells in the body, the structure of sperm cells speaks to their function. Sperm have a distinctive head, mid-piece, and tail region (Figure \(\PageIndex{5}\)). The head of the sperm contains the extremely compact haploid nucleus with very little cytoplasm. These qualities contribute to the overall small size of the sperm (the head is only 5 μ m long). A structure called the acrosome covers most of the head of the sperm cell as a “cap” that is filled with lysosomal enzymes important for preparing sperm to participate in fertilization. Tightly packed mitochondria fill the mid-piece of the sperm. ATP produced by these mitochondria will power the flagellum, which extends from the neck and the mid-piece through the tail of the sperm, enabling it to move the entire sperm cell. The central strand of the flagellum, the axial filament, is formed from one centriole inside the maturing sperm cell during the final stages of spermatogenesis.

Sperm Transport
To fertilize an egg, sperm must be moved from the seminiferous tubules in the testes, through the epididymis, and—later during ejaculation—along the length of the penis and out into the female reproductive tract.
Role of the Epididymis
From the lumen of the seminiferous tubules, the immotile sperm are surrounded by testicular fluid and moved to the epididymis (plural = epididymides), a coiled tube attached to the testis where newly formed sperm continue to mature (see Figure \(\PageIndex{3}\)). Though the epididymis does not take up much room in its tightly coiled state, it would be approximately 6 m (20 feet) long if straightened. It takes an average of 12 days for sperm to move through the coils of the epididymis, with the shortest recorded transit time in humans being one day. Sperm enter the head of the epididymis and are moved along predominantly by the contraction of smooth muscles lining the epididymal tubes. As they are moved along the length of the epididymis, the sperm further mature and acquire the ability to move under their own power. Once inside the female reproductive tract, they will use this ability to move independently toward the unfertilized egg. The more mature sperm are then stored in the tail of the epididymis (the final section) until ejaculation occurs.
Duct System
During ejaculation, sperm exit the tail of the epididymis and are pushed by smooth muscle contraction to the ductus deferens (also called the vas deferens). The ductus deferens is a thick, muscular tube that is bundled together inside the scrotum with connective tissue, blood vessels, and nerves into a structure called the spermatic cord (see Figure \(\PageIndex{1}\) and Figure \(\PageIndex{2}\)). Because the ductus deferens is physically accessible within the scrotum, surgical sterilization to interrupt sperm delivery can be performed by cutting and sealing a small section of the ductus (vas) deferens. This procedure is called a vasectomy, and it is an effective form of male birth control. Although it may be possible to reverse a vasectomy, clinicians consider the procedure permanent, and advise men to undergo it only if they are certain they no longer wish to father children.
Watch this video to learn about a vasectomy. As described in this video, a vasectomy is a procedure in which a small section of the ductus (vas) deferens is removed from the scrotum. This interrupts the path taken by sperm through the ductus deferens. If sperm do not exit through the vas, either because the man has had a vasectomy or has not ejaculated, in what region of the testis do they remain?
From each epididymis, each ductus deferens extends superiorly into the abdominal cavity through the inguinal canal in the abdominal wall. From here, the ductus deferens continues posteriorly to the pelvic cavity, ending posterior to the bladder where it dilates in a region called the ampulla (meaning “flask”).
Sperm make up only 5 percent of the final volume of semen , the thick, milky fluid that the male ejaculates. The bulk of semen is produced by three critical accessory glands of the male reproductive system: the seminal vesicles, the prostate, and the bulbourethral glands.

Seminal Vesicles
As sperm pass through the ampulla of the ductus deferens at ejaculation, they mix with fluid from the associated seminal vesicle (see Figure \(\PageIndex{1}\)). The paired seminal vesicles are glands that contribute approximately 60 percent of the semen volume. Seminal vesicle fluid contains large amounts of fructose, which is used by the sperm mitochondria to generate ATP to allow movement through the female reproductive tract.
The fluid, now containing both sperm and seminal vesicle secretions, next moves into the associated ejaculatory duct , a short structure formed from the ampulla of the ductus deferens and the duct of the seminal vesicle. The paired ejaculatory ducts transport the seminal fluid into the next structure, the prostate gland.
Prostate Gland
As shown in Figure \(\PageIndex{1}\), the centrally located prostate gland sits anterior to the rectum at the base of the bladder surrounding the prostatic urethra (the portion of the urethra that runs within the prostate). About the size of a walnut, the prostate is formed of both muscular and glandular tissues. It excretes an alkaline, milky fluid to the passing seminal fluid—now called semen—that is critical to first coagulate and then decoagulate the semen following ejaculation. The temporary thickening of semen helps retain it within the female reproductive tract, providing time for sperm to utilize the fructose provided by seminal vesicle secretions. When the semen regains its fluid state, sperm can then pass farther into the female reproductive tract.
The prostate normally doubles in size during puberty. At approximately age 25, it gradually begins to enlarge again. This enlargement does not usually cause problems; however, abnormal growth of the prostate, or benign prostatic hyperplasia (BPH), can cause constriction of the urethra as it passes through the middle of the prostate gland, leading to a number of lower urinary tract symptoms, such as a frequent and intense urge to urinate, a weak stream, and a sensation that the bladder has not emptied completely. By age 60, approximately 40 percent of men have some degree of BPH. By age 80, the number of affected individuals has jumped to as many as 80 percent. Treatments for BPH attempt to relieve the pressure on the urethra so that urine can flow more normally. Mild to moderate symptoms are treated with medication, whereas severe enlargement of the prostate is treated by surgery in which a portion of the prostate tissue is removed.
Another common disorder involving the prostate is prostate cancer. According to the Centers for Disease Control and Prevention (CDC), prostate cancer is the second most common cancer in men. However, some forms of prostate cancer grow very slowly and thus may not ever require treatment. Aggressive forms of prostate cancer, in contrast, involve metastasis to vulnerable organs like the lungs and brain. There is no link between BPH and prostate cancer, but the symptoms are similar. Prostate cancer is detected by a medical history, a blood test, and a rectal exam that allows physicians to palpate the prostate and check for unusual masses. If a mass is detected, the cancer diagnosis is confirmed by biopsy of the cells.
Bulbourethral Glands
The final addition to semen is made by two bulbourethral glands (or Cowper’s glands) that release a thick, salty fluid that lubricates the end of the urethra and the vagina, and helps to clean urine residues from the penile urethra. The fluid from these accessory glands is released after the male becomes sexually aroused, and shortly before the release of the semen. It is therefore sometimes called pre-ejaculate. It is important to note that, in addition to the lubricating proteins, it is possible for bulbourethral fluid to pick up sperm already present in the urethra, and therefore it may be able to cause pregnancy.
Watch this video to explore the structures of the male reproductive system and the path of sperm, which starts in the testes and ends as the sperm leave the penis through the urethra. Where are sperm deposited after they leave the ejaculatory duct,
The penis is the male organ of copulation (sexual intercourse). It is flaccid for non-sexual actions, such as urination, and turgid and rod-like with sexual arousal. When erect, the stiffness of the organ allows it to penetrate into the vagina and deposit semen into the female reproductive tract.

The shaft of the penis surrounds the urethra (Figure \(\PageIndex{6}\)). The shaft is composed of three column-like chambers of erectile tissue that span the length of the shaft. Each of the two larger lateral chambers is called a corpus cavernosum (plural = corpora cavernosa). Together, these make up the bulk of the penis. The corpus spongiosum , which can be felt as a raised ridge on the erect penis, is a smaller chamber that surrounds the spongy, or penile, urethra. The end of the penis, called the glans penis , has a high concentration of nerve endings, resulting in very sensitive skin that influences the likelihood of ejaculation (see Figure \(\PageIndex{1}\)). The skin from the shaft extends down over the glans and forms a collar called the prepuce (or foreskin). The foreskin also contains a dense concentration of nerve endings, and both lubricate and protect the sensitive skin of the glans penis. A surgical procedure called circumcision, often performed for religious or social reasons, removes the prepuce, typically within days of birth.
Both sexual arousal and REM sleep (during which dreaming occurs) can induce an erection. Penile erections are the result of vasocongestion, or engorgement of the tissues because of more arterial blood flowing into the penis than is leaving in the veins. During sexual arousal, nitric oxide (NO) is released from nerve endings near blood vessels within the corpora cavernosa and spongiosum. Release of NO activates a signaling pathway that results in relaxation of the smooth muscles that surround the penile arteries, causing them to dilate. This dilation increases the amount of blood that can enter the penis and induces the endothelial cells in the penile arterial walls to also secrete NO and perpetuate the vasodilation. The rapid increase in blood volume fills the erectile chambers, and the increased pressure of the filled chambers compresses the thin-walled penile venules, preventing venous drainage of the penis. The result of this increased blood flow to the penis and reduced blood return from the penis is erection. Depending on the flaccid dimensions of a penis, it can increase in size slightly or greatly during erection, with the average length of an erect penis measuring approximately 15 cm.
DISORDERS OF THE Male Reproductive System
Erectile dysfunction (ED) is a condition in which a man has difficulty either initiating or maintaining an erection. The combined prevalence of minimal, moderate, and complete ED is approximately 40 percent in men at age 40, and reaches nearly 70 percent by 70 years of age. In addition to aging, ED is associated with diabetes, vascular disease, psychiatric disorders, prostate disorders, the use of some drugs such as certain antidepressants, and problems with the testes resulting in low testosterone concentrations. These physical and emotional conditions can lead to interruptions in the vasodilation pathway and result in an inability to achieve an erection.
Recall that the release of NO induces relaxation of the smooth muscles that surround the penile arteries, leading to the vasodilation necessary to achieve an erection. To reverse the process of vasodilation, an enzyme called phosphodiesterase (PDE) degrades a key component of the NO signaling pathway called cGMP. There are several different forms of this enzyme, and PDE type 5 is the type of PDE found in the tissues of the penis. Scientists discovered that inhibiting PDE5 increases blood flow, and allows vasodilation of the penis to occur.
PDEs and the vasodilation signaling pathway are found in the vasculature in other parts of the body. In the 1990s, clinical trials of a PDE5 inhibitor called sildenafil were initiated to treat hypertension and angina pectoris (chest pain caused by poor blood flow through the heart). The trial showed that the drug was not effective at treating heart conditions, but many men experienced erection and priapism (erection lasting longer than 4 hours). Because of this, a clinical trial was started to investigate the ability of sildenafil to promote erections in men suffering from ED. In 1998, the FDA approved the drug, marketed as Viagra®. Since approval of the drug, sildenafil and similar PDE inhibitors now generate over a billion dollars a year in sales, and are reported to be effective in treating approximately 70 to 85 percent of cases of ED. Importantly, men with health problems—especially those with cardiac disease taking nitrates—should avoid Viagra or talk to their physician to find out if they are a candidate for the use of this drug, as deaths have been reported for at-risk users.
Testosterone
Testosterone, an androgen, is a steroid hormone produced by Leydig cells . The alternate term for Leydig cells, interstitial cells, reflects their location between the seminiferous tubules in the testes. In male embryos, testosterone is secreted by Leydig cells by the seventh week of development, with peak concentrations reached in the second trimester. This early release of testosterone results in the anatomical differentiation of the male sexual organs. In childhood, testosterone concentrations are low. They increase during puberty, activating characteristic physical changes and initiating spermatogenesis.
Functions of Testosterone
The continued presence of testosterone is necessary to keep the male reproductive system working properly, and Leydig cells produce approximately 6 to 7 mg of testosterone per day. Testicular steroidogenesis (the manufacture of androgens, including testosterone) results in testosterone concentrations that are 100 times higher in the testes than in the circulation. Maintaining these normal concentrations of testosterone promotes spermatogenesis, whereas low levels of testosterone can lead to infertility. In addition to intratesticular secretion, testosterone is also released into the systemic circulation and plays an important role in muscle development, bone growth, the development of secondary sex characteristics, and maintaining libido (sex drive) in both males and females. In females, the ovaries secrete small amounts of testosterone, although most is converted to estradiol. A small amount of testosterone is also secreted by the adrenal glands in both sexes.
AGING AND THE Male Reproductive System
Declines in Leydig cell activity can occur in men beginning at 40 to 50 years of age. The resulting reduction in circulating testosterone concentrations can lead to symptoms of andropause, also known as male menopause. While the reduction in sex steroids in men is akin to female menopause, there is no clear sign—such as a lack of a menstrual period—to denote the initiation of andropause. Instead, men report feelings of fatigue, reduced muscle mass, depression, anxiety, irritability, loss of libido, and insomnia. A reduction in spermatogenesis resulting in lowered fertility is also reported, and sexual dysfunction can also be associated with andropausal symptoms.
Whereas some researchers believe that certain aspects of andropause are difficult to tease apart from aging in general, testosterone replacement is sometimes prescribed to alleviate some symptoms. Recent studies have shown a benefit from androgen replacement therapy on the new onset of depression in elderly men; however, other studies caution against testosterone replacement for long-term treatment of andropause symptoms, showing that high doses can sharply increase the risk of both heart disease and prostate cancer.
Chapter Review
Gametes are the reproductive cells that combine to form offspring. Organs called gonads produce the gametes, along with the hormones that regulate human reproduction. The male gametes are called sperm. Spermatogenesis, the production of sperm, occurs within the seminiferous tubules that make up most of the testis. The scrotum is the muscular sac that holds the testes outside of the body cavity.
Spermatogenesis begins with mitotic division of spermatogonia (stem cells) to produce primary spermatocytes that undergo the two divisions of meiosis to become secondary spermatocytes, then the haploid spermatids. During spermiogenesis, spermatids are transformed into spermatozoa (formed sperm). Upon release from the seminiferous tubules, sperm are moved to the epididymis where they continue to mature. During ejaculation, sperm exit the epididymis through the ductus deferens, a duct in the spermatic cord that leaves the scrotum. The ampulla of the ductus deferens meets the seminal vesicle, a gland that contributes fructose and proteins, at the ejaculatory duct. The fluid continues through the prostatic urethra, where secretions from the prostate are added to form semen. These secretions help the sperm to travel through the urethra and into the female reproductive tract. Secretions from the bulbourethral glands protect sperm and cleanse and lubricate the penile (spongy) urethra.
The penis is the male organ of copulation. Columns of erectile tissue called the corpora cavernosa and corpus spongiosum fill with blood when sexual arousal activates vasodilatation in the blood vessels of the penis. Testosterone regulates and maintains the sex organs and sex drive, and induces the physical changes of puberty. Interplay between the testes and the endocrine system precisely control the production of testosterone with a negative feedback loop.
Review Questions
Q. What are male gametes called?
D. testosterone
Q. Leydig cells ________.
A. secrete testosterone
B. activate the sperm flagellum
C. support spermatogenesis
D. secrete seminal fluid
Q. Which hypothalamic hormone contributes to the regulation of the male reproductive system?
A. luteinizing hormone
B. gonadotropin-releasing hormone
C. follicle-stimulating hormone
D. androgens
Q. What is the function of the epididymis?
A. sperm maturation and storage
B. produces the bulk of seminal fluid
C. provides nitric oxide needed for erections
D. spermatogenesis
Q. Spermatogenesis takes place in the ________.
A. prostate gland
B. glans penis
C. seminiferous tubules
D. ejaculatory duct
Critical Thinking Questions
Q. Briefly explain why mature gametes carry only one set of chromosomes.
A. A single gamete must combine with a gamete from an individual of the opposite sex to produce a fertilized egg, which has a complete set of chromosomes and is the first cell of a new individual.
Q. What special features are evident in sperm cells but not in somatic cells, and how do these specializations function?
A. Unlike somatic cells, sperm are haploid. They also have very little cytoplasm. They have a head with a compact nucleus covered by an acrosome filled with enzymes, and a mid-piece filled with mitochondria that power their movement. They are motile because of their tail, a structure containing a flagellum, which is specialized for movement.
Q. What do each of the three male accessory glands contribute to the semen?
A. The three accessory glands make the following contributions to semen: the seminal vesicle contributes about 60 percent of the semen volume, with fluid that contains large amounts of fructose to power the movement of sperm; the prostate gland contributes substances critical to sperm maturation; and the bulbourethral glands contribute a thick fluid that lubricates the ends of the urethra and the vagina and helps to clean urine residues from the urethra.
Q. Describe how penile erection occurs.
A. During sexual arousal, nitric oxide (NO) is released from nerve endings near blood vessels within the corpora cavernosa and corpus spongiosum. The release of NO activates a signaling pathway that results in relaxation of the smooth muscles that surround the penile arteries, causing them to dilate. This dilation increases the amount of blood that can enter the penis, and induces the endothelial cells in the penile arterial walls to secrete NO, perpetuating the vasodilation. The rapid increase in blood volume fills the erectile chambers, and the increased pressure of the filled chambers compresses the thin-walled penile venules, preventing venous drainage of the penis. An erection is the result of this increased blood flow to the penis and reduced blood return from the penis.
Q. While anabolic steroids (synthetic testosterone) bulk up muscles, they can also affect testosterone production in the testis. Using what you know about negative feedback, describe what would happen to testosterone production in the testis if a male takes large amounts of synthetic testosterone.
A. Testosterone production by the body would be reduced if a male were taking anabolic steroids. This is because the hypothalamus responds to rising testosterone levels by reducing its secretion of GnRH, which would in turn reduce the anterior pituitary’s release of LH, finally reducing the manufacture of testosterone in the testes.
Contributors and Attributions
OpenStax Anatomy & Physiology (CC BY 4.0). Access for free at https://openstax.org/books/anatomy-and-physiology
Human Physiology/The male reproductive system
Homeostasis — Cells — Integumentary — Nervous — Senses — Muscular — Blood — Cardiovascular — Immune — Urinary — Respiratory — Gastrointestinal — Nutrition — Endocrine — Reproduction (male) — Reproduction (female) — Pregnancy — Genetics — Development — Answers
- 1 Introduction
- 2.2 Epididymis
- 2.3 Ductus Deferens
- 2.4 Seminal Vesicles
- 2.5 Ejaculatory Ducts
- 2.6 Prostate Gland
- 2.7 Bulbourethral Glands
- 2.9 Urethra
- 2.10 Overview of Male Reproductive System Structure and Function
- 2.11 Composition of human semen
- 3.1 Hormone Regulation
- 3.2 Erection
- 3.3 Ejaculation
- 3.4 Sperm Production
- 3.5 Sperm Pathway
- 4.1 Testicular size, function, and fertility
- 4.2 Genitalia
- 4.3 Genital Erection
- 4.4 Pubic hair in boys
- 5 Sexual Homology
- 7.1 Disorders of Penis
- 7.2 Contraceptive for Men
- 8 Review Questions
- 11 References
Introduction [ edit | edit source ]
In simple terms, reproduction is the process by which organisms create descendants. This miracle is a characteristic that all living things have in common and sets them apart from nonliving things. But even though the reproductive system is essential to keeping a species alive, it is not essential to keeping an individual alive.
In human reproduction, two kinds of sex cells or gametes are involved. Sperm, the male gamete, and a secondary oocyte (along with first polar body and corona radiata), the male gamete must meet in the female reproductive system to create a new individual. For reproduction to occur, both the female and male reproductive systems are essential. It is a common misnomer to refer to a woman's gametic cell as an egg or ovum , but this is impossible. A secondary oocyte must be fertilized by the male gamete before it becomes an "ovum" or "egg".
While both the female and male reproductive systems are involved with producing, nourishing and transporting either the oocyte or sperm , they are different in shape and structure. The male has reproductive organs, or genitals, that are both inside and outside the pelvis, while the female has reproductive organs entirely within the pelvis.
The male reproductive system consists of the testes and a series of ducts and glands. Sperm are produced in the testes and are transported through the reproductive ducts. These ducts include the epididymis, vas deferens, ejaculatory duct and urethra. The reproductive glands produce secretions that become part of semen, the fluid that is ejaculated from the urethra. These glands include the seminal vesicles, prostate gland, and bulbourethral glands.
Structure [ edit | edit source ]

Testes [ edit | edit source ]
The testes (singular, testis) are located in the scrotum (a sac of skin between the upper thighs). In the male fetus, the testes develop near the kidneys, then descend into the scrotum just before birth. Each testis is about 1 1/2 inches long by 1 inch wide. Testosterone is produced in the testes which stimulates the production of sperm as well as give secondary sex characteristics beginning at puberty.
The two testicles are each held in a fleshy sac called the scrotum. The major function of the scrotal sac is to keep the testes cooler than thirty-seven degrees Celsius (ninety-eight point six degrees Fahrenheit). The external appearance of the scrotum varies at different times in the same individual depending upon temperature and the subsequent contraction or relaxation of two muscles. These two muscles contract involuntarily when it is cold to move the testes closer to the heat of the body in the pelvic region. This causes the scrotum to appear tightly wrinkled. On the contrary, they relax in warm temperatures causing the testes to lower and the scrotum to become flaccid. The temperature of the testes is maintained at about thirty-five degrees Celsius (ninety-five degrees Fahrenheit), which is below normal body temperature. Temperature has to be lower than normal in order for spermatogenesis (sperm production) to take place.

The two muscles that regulate the temperature of the testes are the dartos and cremaster muscles:
- Dartos Muscle
The dartos muscle is a layer of smooth muscle fibers in the subcutaneous tissue of the scrotum (surrounding the scrotum). This muscle is responsible for wrinkling up the scrotum, in conditions of cold weather, in order to maintain the correct temperature for spermatogenesis.
- Cremaster Muscle
The cremaster muscle is a thin strand of skeletal muscle associated with the testes and spermatic cord. This muscle is a continuation of the internal oblique muscle of the abdominal wall, from which it is derived. Seminiferous Tubules
Each testis contains over 100 yards of tightly packed seminiferous tubules. Around 90% of the weight of each testes consists of seminiferous tubules. The seminiferous tubules are the functional units of the testis, where spermatogenesis takes place. Once the sperm are produced, they moved from the seminiferous tubules into the rete testis for further maturation.
Interstitial Cells (Cells of Leydig)
In between the seminiferous tubules within the testes, are instititial cells, or, Cells of Leydig . They are responsible for secreting the male sex hormones (i.e., testosterone).
Sertoli Cells
A Sertoli cell (a kind of sustentacular cell) is a 'nurse' cell of the testes which is part of a seminiferous tubule.
It is activated by follicle-stimulating hormone, and has FSH-receptor on its membranes.
Its main function is to nurture the developing sperm cells through the stages of spermatogenesis. Because of this, it has also been called the "mother cell." It provides both secretory and structural support.
Other functions During the Maturation phase of spermiogenesis, the Sertoli cells consume the unneeded portions of the spermatazoa.
Efferent ductules
The sperm are transported out of the testis and into the epididymis through a series of efferent ductules.
Blood Supply
The testes receive blood through the testicular arteries (gonadal artery). Venous blood is drained by the testicular veins. The right testicular vein drains directly into the inferior vena cava. The left testicular vein drains into the left renal vein.
Epididymis [ edit | edit source ]

The seminiferous tubules join together to become the epididymis. The epididymis is a tube that is about 2 inches that is coiled on the posterior surface of each testis. Within the epididymis the sperm incomplete their maturation (full maturation occur in female genital tract) and their flagella become mobile. This is also a site to store sperm, nourishing them until the next ejaculation. Smooth muscle in the wall of the epididymis propels the sperm into the ductus deferens.
Vasa efferentia from the rete testis open into the epididymis which is a highly coiled tubule. The epididymis has three parts- 1)head or caput epididymis- it is the proximal part of the epididymis. It carries the sperms from the testis. 2)body or corpus epididymis- it the highly convoluted middle part of the epididymis 3)tail or cauda epididymis- it is the last part that takes part in carrying the sperms to the vas deferens. The cauda epididymis continues to form less convoluted vas deferens.
Ductus Deferens [ edit | edit source ]
The ductus (vas) deferens, also called sperm duct, or, spermatic deferens, extends from the epididymis in the scrotum on its own side into the abdominal cavity through the inguinal canal. The inguinal canal is an opening in the abdominal wall for the spermatic cord (a connective tissue sheath that contains the ductus deferens, testicular blood vessels, and nerves. The smooth muscle layer of the ductus deferens contracts in waves of peristalsis during ejaculation.
Seminal Vesicles [ edit | edit source ]
The pair of seminal vesicles are posterior to the urinary bladder. They secrete fructose to provide an energy source for sperm and alkalinity to enhance sperm mobility. The duct of each seminal vesicle joins the ductus deferens on that side to form the ejaculatory duct.
Ejaculatory Ducts [ edit | edit source ]
There are two ejaculatory ducts. Each receives sperm from the ductus deferens and the secretions of the seminal vesicle on its own side. Both ejaculatory ducts empty into the single urethra.
Prostate Gland [ edit | edit source ]
The prostate gland is a muscular gland that surrounds the first inch of the urethra as it emerges from the bladder. The smooth muscle of the prostate gland contracts during ejaculation to contribute to the expulsion of semen from the urethra.
Bulbourethral Glands [ edit | edit source ]

The bulbourethral glands also called Cowper's glands are located below the prostate gland and empty into the urethra. The alkalinity of seminal fluid helps neutralize the acidic vaginal pH and permits sperm mobility in what might otherwise be an unfavorable environment.
Penis [ edit | edit source ]
The penis is an external genital organ. The distal end of the penis is called the glans penis and is covered with a fold of skin called the prepuce or foreskin. Within the penis are masses of erectile tissue. Each consists of a framework of smooth muscle and connective tissue that contains blood sinuses, which are large, irregular vascular channels.
Urethra [ edit | edit source ]
The urethra, which is the last part of the urinary tract, traverses the corpus spongiosum and its opening, known as the meatus, lies on the tip of the glans penis. It is both a passage for urine and for the ejaculation of semen.
Overview of Male Reproductive System Structure and Function [ edit | edit source ]
Composition of human semen [ edit | edit source ].
The components of semen come from two sources: sperm, and "seminal plasma". Seminal plasma, in turn, is produced by contributions from the seminal vesicle, prostate, and bulbourethral glands.
Seminal plasma of humans contains a complex range of organic and inorganic constituents.
The seminal plasma provides a nutritive and protective medium for the spermatozoa during their journey through the female reproductive tract. The normal environment of the vagina is a hostile one for sperm cells, as it is very acidic (from the native microflora producing lactic acid), viscous, and patrolled by immune cells. The components in the seminal plasma attempt to compensate for this hostile environment. Basic amines such as putrescine, spermine, spermidine and cadaverine are responsible for the smell and flavor of semen. These alkaline bases counteract the acidic environment of the vaginal canal, and protect DNA inside the sperm from acidic denaturation.
The components and contributions of semen are as follows:
A 1992 World Health Organization report described normal human semen as having a volume of 2 ml or greater, pH of 7.2 to 8.0, sperm concentration of 20x106 spermatozoa/ml or more, sperm count of 40x106 spermatozoa per ejaculate or more and motility of 50% or more with forward progression (categories a and b) of 25% or more with rapid progression (category a) within 60 minutes of ejaculation. [1]
Functions [ edit | edit source ]
Hormone regulation [ edit | edit source ].
Hormones which control reproduction in males are:
Gonadotropin-Releasing Hormone (GnRH):
- The hypothalamus secretes this hormone into the pituitary gland in the brain.
- There are two gonadotropic hormones, FSH and LH.
Luteinizing Hormone (LH):
- The pituitary gland secretes this hormone after receiving a GnRH signal from the hypothalamus.
- LH stimulates Leydig cells, in the testes, telling them to produce testosterone.
Follicle-Stimulating Hormone (FSH):
- The pituitary gland also secretes this hormone.
- Testosterone helps FSH run through the bloodstream to make Sertoli cells, located in the seminiferous tubules of the testes, to make immature sperm to mature sperm.
Testosterone:
- Also known as "the male hormone" and "androgen".
- Testosterone is vital for the production of sperm.

Erection [ edit | edit source ]
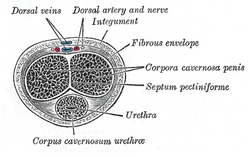
The erection of the penis is its enlarged and firm state. It depends on a complex interaction of psychological, neural, vascular and endocrine factors. The term is also applied to the process that leads to this state.
A penile erection occurs when two tubular structures that run the length of the penis, the corpora cavernosa, become engorged with venous blood. This is a result of parasympathetic nerve induced vasodilation. This may result from any of various physiological stimuli. The corpus spongiosum is a single tubular structure located just below the corpora cavernosa, which contains the urethra, through which urine and semen pass during urination and ejaculation, respectively. This may also become slightly engorged with blood, but less so than the corpora cavernosa.
Penile erection usually results from sexual stimulation and/or arousal, but can also occur by such causes as a full urinary bladder or spontaneously during the course of a day or at night, often during erotic or wet dreams. An erection results in swelling and enlargement of the penis. Erection enables sexual intercourse and other sexual activities (sexual functions), though it is not essential for all sexual activities.
Ejaculation [ edit | edit source ]
Emission is the term used when sperm moves into the urethra. Ejaculation is the term used when sperm is forced out of the urethra and the penis. These are both stimulated by sympathetic nerves.
Sperm Production [ edit | edit source ]
A spermatozoon or spermatozoan (pl. spermatozoa), from the ancient Greek σπέρμα (seed) and ζῷον (living being) and more commonly known as a sperm cell, is the haploid cell that is the male gamete.
Spermatagonia divides several times during the process of sperm development. The entire process of sperm formation and maturation takes about 9-10 weeks. The separate divisions that take place and what happens in each are as follows:
- First division : The first division is done by mitosis, and ensures a constant supply of spermatocytes , each with the diploid number of chromosomes.
- Second division : Spermatocytes then undergo a series of two cell divisions during meiosis to become secondary spermatocytes .
- Third division : Secondary Spermatocytes finally become spermatids . Spermatids, which are haploid cells, mature slowly to become the male gametes, or sperm .
The sperm is the main reproductive cell in males. The sperms differ in that each carry a set of chromosomes dividing each into either a male, or female sperm. The females differ in that they carry a X gene, while the male sperm carry a Y gene. The female sperm also differ phenotypically in that they have a larger head in comparison to the male sperms. This contributes to the male sperm being lighter, and therefore faster and stronger swimmers than their female counterparts (although statistically there is still a 50% chance of an either XY or XX embryo forming.
Spermatozoan stream lines are straight and parallel. The tail flagellates, which we now know propels the sperm cell (at about 1-3 mm/minute in humans) by rotating like a propeller, in a circular motion, not side to side like a whip. The cell is characterized by a minimum of cytoplasm. During fertilization, the sperm's mitochondria gets destroyed by the egg cell, and this means only the mother is able to provide the baby's mitochondria and mitochondrial DNA, which has an important application in tracing maternal ancestry. However it has been recently discovered that mitochondrial DNA can be recombinant.
Spermatozoa are produced in the seminiferous tubules of the testes in a process called spermatogenesis. Round cells called spermatogonia divide and differentiate eventually to become spermatozoa. During copulation the vagina is inseminated, the spermatozoa move through chemotaxis (see glossary) to the ovum inside a Fallopian tube or the uterus.
Sperm Pathway [ edit | edit source ]
Spermatogenesis takes place inside a male’s testes, specifically in the walls of the seminiferous tubules. The epididymis is a tortuously coiled structure topping the testis, it receives immature sperm from the testis and stores it for several days. When ejaculation occurs, sperm is forcefully expelled from the tail of the epididymis into the ductus deferens. Sperm travels through the ductus deferens and up the spermatic cord into the pelvic cavity, over the ureter to the prostate behind the bladder. Here, the vas deferens joins with the seminal vesicle to form the ejaculatory duct, which passes through the prostate and empties into the urethra. Upon the sperm's exit from the testes, into the vas deferens, muscular movements take over. When ejaculation occurs, rhythmic muscle movements of peristalsis propel the sperm forward. This continues throughout the remainder of the sperm's journey through the male reproductive system.
Sperm cells become even more active when they begin to interact with the fertilizing layer of an egg cell. They swim faster and their tail movements become more forceful and erratic. This behavior is called "hyper activation."
A recent discovery links hyper activation to a sudden influx of calcium ions into the tails. The whip-like tail (flagellum) of the sperm is studded with ion channels formed by proteins called CatSper. These channels are selective, allowing only calcium ion to pass. The opening of CatSper channels is responsible for the influx of calcium. The sudden rise in calcium levels causes the flagellum to form deeper bends, propelling the sperm more forcefully through the viscous environment.
The sperm use their tails to push themselves into the epididymis, where they complete their development. It takes sperm about 4 to 6 weeks to travel through the epididymis. The sperm then move to the vas deferens, or sperm duct. The seminal vesicles and prostate gland produce a whitish fluid called seminal fluid, which mixes with sperm to form semen when a male is sexually stimulated.
The penis, which usually hangs limp, becomes hard when a male is sexually excited. Tissues in the penis fill with blood and it becomes stiff and erect (an erection). The rigidity of the erect penis makes it easier to insert into the female's vagina during sexual intercourse, and the extended length allows it to reach deeper into the female's oviduct , the passage from the ovaries to the outside of the body (allowing a shorter travel distance for the spermatozoa).
When the erect penis is stimulated to orgasm, muscles around the reproductive organs contract and force the semen through the duct system and urethra. Semen is pushed out of the male's body through his urethra - ejaculation. The speed of the semen is about 70 mph when ejaculation comes and it can contain 100 to 600 million sperm cells. When the male ejaculates during intercourse, semen is deposited into the fornix at the base of the female's vagina, near the cervix. From the fornix, the sperm make their way up through the cervix and move through the uterus with help from uterine contractions.
Sperm hyperactivity is necessary for breaking through two physical barriers that protect the egg from fertilization. The first barrier to sperm is made up of so-called cumulus cells embedded in a gel-like substance made primarily of hyaluronic acid. The cumulus cells develop in the ovary with the egg and support it as it grows.
The second barrier coating the oocyte is a thick shell formed by glycoproteins called the zona pellucida. One of the proteins that make up the zona pellucida binds to a partner molecule on the sperm. This lock-and-key type mechanism is species-specific and prevents the sperm and egg of different species from fusing. There is some evidence that this binding is what triggers the acrosome to release the enzymes that allow the sperm to fuse with the egg.
When a sperm cell reaches the egg the acrosome releases its enzymes. These enzymes weaken the shell, allowing the sperm cell to penetrate it and reach the plasma membrane of the egg. Part of the sperm's cell membrane then fuses with the egg cell's membrane, and the sperm cell sinks into the egg (at which point the sperm tail falls off).
Upon penetration, the egg cell membrane undergoes a change and becomes impenetrable, preventing further fertilization.
The binding of the sperm to an ovum is called a zygote. A zygote is a single cell, with a complete set of chromosomes, that normally develops into an embryo.
Puberty [ edit | edit source ]
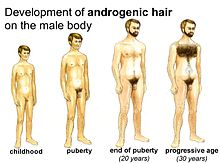
In addition to producing sperm, the male reproductive system also produces sex hormones, which help a boy develop into a sexually mature man during puberty. When a baby boy is born, he has all the parts of his reproductive system in place, but it isn't until puberty that his reproductive organs mature and become fully functional. As an newborn FSH and LH levels are high and after a few weeks levels drop to extremely low. When puberty begins, usually between the ages of 10 and 14, the pituitary gland - which is located in the brain - secretes hormones that stimulate the testicles to produce testosterone. The production of testosterone brings about many physical changes. Although the timing of these changes is different for each individual male, the stages of puberty generally follow a set sequence.
- First stage: the scrotum and testes grow larger, the apocrine glands develop (see explanation of apocrine glands in glossary).
- Second stage: the penis becomes longer, and the seminal vesicles and prostate gland grow. Hair begins to grow in the pubic region. Reproductive capacity has usually developed by this stage.
- Third stage: hair begins to appear on the face and underarms. During this time, a male's voice also deepens. Fertility continues to increase.
Testicular size, function, and fertility [ edit | edit source ]
In boys, testicular enlargement is the first physical manifestation of puberty (and is termed gonadarche). Testes in prepubertal boys change little in size from about 1 year of age to the onset of puberty, averaging about 2–3 cc in volume and about 1.5-2 cm in length. Testicular size continues to increase throughout puberty, reaching maximal adult size about 6 years later. While 18-20 cc is reportedly an average adult size, there is wide variation in the normal population.
The testes have two primary functions: to produce hormones and to produce sperm. The Leydig cells produce testosterone (as described below), which in turn produces most of the changes of male puberty. However, most of the increasing bulk of testicular tissue is spermatogenic tissue (primarily Sertoli and interstitial cells). The development of sperm production and fertility in males is not as well researched. Sperm can be detected in the morning urine of most boys after the first year of pubertal changes (and occasionally earlier).
Genitalia [ edit | edit source ]
A boy's penis grows little from the fourth year of life until puberty. Average prepubertal penile length is 4 cm. The prepubertal genitalia are described as stage 1. Within months after growth of the testes begins, rising levels of testosterone promote growth of the penis and scrotum. This earliest discernible beginning of pubertal growth of the genitalia is referred to as stage 2. The penis continues to grow until about 18 years of age, reaching an average adult size of about 10-16 cm.
Although erections and orgasm can occur in prepubertal boys, they become much more common during puberty, accompanied by development of libido (sexual desire). Ejaculation becomes possible early in puberty; prior to this boys may experience dry orgasms. Emission of seminal fluid may occur due to masturbation or spontaneously during sleep (commonly termed a wet dream , and more clinically called a nocturnal emission ). The ability to ejaculate is a fairly early event in puberty compared to the other characteristics, and can occur even before reproductive capacity itself. In parallel to the irregularity of the first few periods of a girl, for the first one or two years after a boy's first ejaculation, his seminal fluid may contain few active sperm.
If the foreskin of a boy does not become retractable during childhood, it normally begins to retract during puberty. This occurs as a result of the increased production of testosterone and other hormones in the body.

Genital Erection [ edit | edit source ]
The penis contains two chambers called the corpora cavernosa, which run the length of the organ. A spongy tissue, full of muscle, veins, arteries, etc. fills these chambers. The corpora cavernosa are surrounded by a membrane, called the tunica albuginea.
Erection begins with sensory or mental stimulation, or both. Impulses from the brain and local nerves cause the muscles of the corpora cavernosa to relax, allowing blood to flow in and fill the spaces. The blood creates pressure in the corpora cavernosa, making the penis expand. The tunica albuginea helps trap the blood in the corpora cavernosa, thereby sustaining erection. When muscles in the penis contract to stop the inflow of blood and open outflow channels, erection is reversed.
Pubic hair in boys [ edit | edit source ]
Pubic hair often appears on a boy shortly after the genitalia begin to grow. As in girls, the first appearance of pubic hair is termed pubarche and the pubic hairs are usually first visible at the dorsal (abdominal) base of the penis. The first few hairs are described as stage 2. Stage 3 is usually reached within another 6 to 12 months, when the hairs are too numerous to count. By stage 4, the pubic hairs densely fill the "pubic triangle." Stage 5 refers to spread of pubic hair to the inner thighs and upward towards the umbilicus as part of the developing abdominal hair.
Sexual Homology [ edit | edit source ]
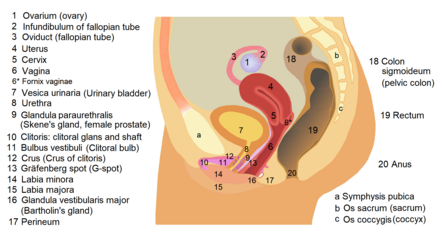
In short, this is a known list of sex organs that evolve from the same tissue in a human life.
Aging [ edit | edit source ]
For most men, testosterone secretion continues throughout life, as does sperm production, though both diminish with advancing age. Probably the most common reproductive problem for older men is prostatic hypertrophy, enlargement of the prostate gland. This causes the urethra to compress and urination becomes difficult. Residual urine in the bladder increases the chance of urinary tract infections. Prostate hypertrophy is usually benign, but cancer of the prostate is one of the more common cancers in elderly men. A TURP is commonly used to correct this problem if the symptoms do not improve in response to home treatment and medication.
Erectile dysfunction (ED) is another common problem seen in aging males. In older men, ED usually has a physical cause, such as disease, injury, or side effects of drugs. Any disorder that impairs blood flow in the penis or causes injury to the nerves has the potential to cause ED. Although it is not an inevitable part of aging, incidences increases with age: About 5 percent of 40-year-old men and between 15 and 25 percent of 65-year-old men experience ED. As discouraging as Erectile dysfunction may be, it is treatable at any age, and awareness of this fact has been growing. More men have been seeking help and returning to normal sexual activity because of improved, successful treatments for ED.
Things that can go wrong with the male reproductive system [ edit | edit source ]
Boys may sometimes experience reproductive system problems. Below are some examples of disorders that affect the male reproductive system (Disorders of the Scrotum, Testicles, or Epididymis). Conditions affecting the scrotal contents may involve the testicles, epididymis, or the scrotum itself.
- Testicular trauma. Even a mild injury to the testicles can cause severe pain, bruising, or swelling. Most testicular injuries occur when the testicles are struck, hit, kicked, or crushed, usually during sports or due to other trauma. Testicular torsion, when 1 of the testicles twists around, cutting off the blood supply, is also a problem that some teen males experience - although it's not common. Surgery is needed to untwist the cord and save the testicle.
- Varicocele . This is a varicose vein (an abnormally swollen vein) in the network of veins that run from the testicles. Varicoceles commonly develop while a boy is going through puberty. A varicocele is usually not harmful, although in some people it may damage the testicle or decrease sperm production, so it helps for you to take your child to see his doctor if he is concerned about changes in his testicles.
- Testicular cancer . This is one of the most common cancers in men younger than 40. It occurs when cells in the testicle divide abnormally and form a tumor. Testicular cancer can spread to other parts of the body, but if it's detected early, the cure rate is excellent. Teen boys should be encouraged to learn to perform testicular self-examinations.
- Epididymitis is inflammation of the epididymis, the coiled tubes that connect the testes with the vas deferens. It is usually caused by an infection, such as the sexually transmitted disease chlamydia, and results in pain and swelling next to 1 of the testicles.
- Hydrocele . A hydrocele occurs when fluid collects in the membranes surrounding the testes. Hydroceles may cause swelling of the testicle but are generally painless. In some cases, surgery may be needed to correct the condition.
- Inguinal hernia . When a portion of the intestines pushes through an abnormal opening or weakening of the abdominal wall and into the groin or scrotum, it is known as an inguinal hernia. The hernia may look like a bulge or swelling in the groin area. It can be corrected with surgery.
Disorders of Penis [ edit | edit source ]
Disorders of the Penis Disorders affecting the penis include the following:
- Inflammation of the penis. Symptoms of penile inflammation include redness, itching, swelling, and pain. Balanitis occurs when the glans (the head of the penis) becomes inflamed. Posthitis is foreskin inflammation, which is usually due to a yeast or bacterial infection.
- Hypospadias. This is a disorder in which the urethra opens on the underside of the penis, not at the tip.
- Phimosis. This is a tightness of the foreskin of the penis and is common in newborns and young children. It usually resolves itself without treatment. If it interferes with urination, circumcision (removal of the foreskin) may be recommended.
- Paraphimosis. This may develop when a boy's uncircumcised penis is retracted but doesn't return to the unretracted position. As a result, blood flow to the penis may be impaired, and your child may experience pain and swelling. A doctor may try to use lubricant to make a small incision so the foreskin can be pulled forward. If that doesn't work, circumcision may be recommended.
- Ambiguous genitalia. This occurs when a child is born with genitals that aren't clearly male or female. In most boys born with this disorder, the penis may be very small or nonexistent, but testicular tissue is present. In a small number of cases, the child may have both testicular and ovarian tissue.
- Micro penis. This is a disorder in which the penis, although normally formed, is well below the average size, as determined by standard measurements.
- Sexually transmitted diseases. Sexually transmitted diseases (STDs) that can affect boys include human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS), human papillomavirus (HPV, or genital warts), syphilis, chlamydia, gonorrhea, genital herpes, and hepatitis B. They are spread from one person to another mainly through sexual intercourse.
- Erectile dysfunction. E.D. is the inability to get or keep an erection firm enough for sexual intercourse. This can also called impotence. The word "impotence" may also be used to describe other problems that can interfere with sexual intercourse and reproduction, such as problems with ejaculation or orgasm and lack of sexual desire. Using the term erectile dysfunction clarifies that those other problems are not involved.
Contraceptive for Men [ edit | edit source ]
Vasectomy: In the procedure the vas deferens of each testes is cut and tied off to prevent the passage of sperm. Sperm is still produced and stored in crypt sites causing inflammation. Because of this inflammatory response the immune system acts on them destroying them and then having antisperm antibodies. This causes a lower possibility if the vasectomy is reversed to becoming fertile again.
Condoms: A device, usually made of latex, or more recently polyurethane, that is used during sexual intercourse. It is put on a man's penis and physically blocks ejaculated semen from entering the body of a sexual partner. Condoms are used to prevent pregnancy, transmission of sexually transmitted diseases (STDs - such as gonorrhea, syphilis, and HIV), or both.
Review Questions [ edit | edit source ]
1. This is needed to make immature sperm mature
2. These become engorged with blood in an erection
3. The difference between male and female sperm
4. The entire process of sperm formation takes about
5. Hyper Activation occurs when
6. It takes sperm ___________ weeks to travel through the epididymis
7. While singing in the choir, Ben suddenly notices his voice is constantly cracking. This is caused by
8. In sexual homology, the glans penis in the male is equal to _____________ in the female
9. In sexual homology, the ___________ in the male is equal to the fallopian tubes in the female
10. Joe has a bulge in the groin area that seems to get worse when he lifts things. This most likely is
Glossary [ edit | edit source ]
Androgen : The generic term for any natural or synthetic compound, usually a steroid hormone, that stimulates or controls the development and maintenance of masculine characteristics in vertebrates by binding to androgen receptors. This includes the activity of the accessory male sex organs and development of male secondary sex characteristics. They are also the precursor of all estrogens, the female sex hormones. The primary and most well-known androgen is testosterone.
Apocrine Glands : Apocrine sweat glands develop during the early to mid puberty ages approximately around the age of 15 and release more than normal amounts of sweat for approximately a month and subsequently regulate and release normal amounts of sweat after a certain period of time. They are located wherever there is body hair. These glands produce sweat that contains fatty materials. Mainly present in the armpits and around the genital area, their activity is the main cause of sweat odor, due to the bacteria that break down the organic compounds in the sweat.
Bulbourethral Glands : male accessory sex glands that secrete mucus for lubrication
Chemotaxis : Chemotaxis is a kind of taxis, in which bodily cells, bacteria, and other single-cell or multicellular organisms direct their movements according to certain chemicals in their environment. This is important for bacteria to find food (for example, glucose) by swimming towards the highest concentration of food molecules, or to flee from poisons (for example, phenol). In multicellular organisms, chemotaxis is critical to development as well as normal function. In addition, it has been recognized that mechanisms that allow chemotaxis in animals can be subverted during cancer metastasis.
Corpora Cavernosa : one of a pair of a sponge-like regions of erectile tissue which contain most of the blood in the male penis during erection
Ductus Deferens : epididymal ducts from each testis converge to form a large, thick walled, muscular duct
Ejaculatory Ducts : two ducts, receive sperm from the ductus deferens and secretions from the seminal vesicle; the ducts then empty into the urethra
Epididymis : comma shaped and loosely attached to the rear surface of each testis
Erectile Tissue : smooth muscle and connective tissue inside the penis that contain blood sinuses; large, irregular vascular channels
Erection : the penis at its enlarged and firm state; occurs when the corpora cavernosa become engorged with venous blood
Flagellum : the whip-like tail of a sperm, propels the sperm towards the egg in hopes of achieving fertilization
Follicle-Stimulating Hormone (FSH) : hormone that stimulates production of sertoli cells, to make immature sperm to mature sperm
Glans Penis : distal end of the penis, covered with the foreskin
Gonadotropin-Releasing Hormone (GnRH) : hormone secreted by the hypothalamus into the pituitary gland; two types, FSH and LH
Libido : In its common usage, it means sexual desire; however, more technical definitions, such as those found in the work of Carl Jung, are more general, referring to libido as the free creative—or psychic—energy an individual has to put toward personal development, or individuation.
Luteinizing Hormone (LH) : hormone that stimulates Leydig cells in the testes to produce testosterone
Oviduct : the passage in females from the ovaries to the outside of the body.
Penis : external genital organ of the male
Prostate Gland : male accessory sex gland that secretes an alkaline fluid, which neutralizes acidic vaginal secretions
Puberty : the period of maturation and arousal of the dormant and nonfunctional reproductive system; usually occurs in males between the ages of 10 and 15
Scrotum : skin covered sac that houses the male testicles; keeps the testicles away from the body so that they can stay a few degrees cooler than the body, for better sperm production
Seminal Vesicle : male accessory sex glands that supply fructose to ejaculated sperm and secrete prostaglandins
Seminiferous Tubules : highly coiled tubules within the testes that produce spermatozoa
Sertoli Cell : A Sertoli cell (a kind of sustentacular cell) is a 'nurse' cell of the testes which is part of a seminiferous tubule.
Sexual Homology : sex organs that evolve from the same tissues in both male and females
Sperm : main reproductive cell in males
Spermatogenesis : sperm production
Testes : located in the scrotum, produces testosterone which stimulates production of sperm
Testosterone : male sex hormone secreted by the leydig cells of the testes, vital for the production of sperm
TURP : transurethral resection of the prostate. During TURP, an instrument is inserted up the urethra to remove the section of the prostate that is blocking urine flow. This is most commonly caused by benign prostatic hyperplasia (BPH). A TURP usually requires hospitalization and is done using a general or spinal anesthetic. It is now the most common surgery used to remove part of an enlarged prostate.
Urethra : the last part of the urinary tract; in males, it is the passage for both urine and sperm
Varicocele : varicose vein of the testicles, sometimes a cause of male infertility
Vasectomy : most common sterilization procedure in males; small segment of each ductus deferens is surgically removed after it passes from the testis
Summary [ edit | edit source ]
Both male and female reproductive systems may seem somewhat isolated from other body systems in that their purpose is to create new life and not just to maintain existing life. There are however significant relationships between the reproductive system and other body systems. All systems relate in one way or another to help our bodies maintain homeostasis.
References [ edit | edit source ]
- "Essentials of Anatomy and Physiology" by Valerie C. Scanlon and Tina Sanders
- "Web MD": http://www.webmd.com
- Wikibook: Sexual Health
- ↑ Male Infertility from A to Z: A Concise Encyclopedia . Google books
- Book:Human Physiology
Navigation menu
All about sperm
The Ultimate Guide to Understanding the Pathway of Sperm: A Fascinating Journey [Infographic Included]

What is Pathway of Sperm?
How does the pathway of sperm work explained step by step, frequently asked questions about the pathway of sperm, top 5 facts to know about the pathway of sperm, navigating the complex pathway of sperm: a visual guide, exploring male reproductive anatomy along the pathway of sperm, the importance of a healthy pathway of sperm for fertility and reproduction, table with useful data:, information from an expert, historical fact:.
Table of Contents
The pathway of sperm is the journey that sperm cells take from the testes to the female reproductive tract during fertilization. The journey involves a series of steps, including production, maturation, and transport.
- Sperm cells are produced in the testes through a process called spermatogenesis that begins at puberty and continues throughout life.
- After production, they mature in the epididymis and vas deferens.
- During ejaculation, they pass through the urethra and enter into the female reproductive tract where they swim towards the egg for fertilization.
The process of fertilization is a miraculous event that marks the beginning of new life. The reproductive system of both males and females is responsible for this remarkable achievement. However, the male reproductive system plays a crucial role in fertilization by producing and delivering sperm to the female reproductive system. Sperm are tiny but highly specialized cells that have an incredible journey to traverse before they can reach their ultimate destination – the egg. So how does this process work? Let’s dive into the intricate pathway of sperm step-by-step.
Step 1: Production Spermatogenesis, or the production of sperm, occurs in the seminiferous tubules located within the testes. Under normal conditions, millions of sperm are produced each day through a complex process called meiosis. This is where each diploid cell undergoes two divisions to produce four haploid cells, which are genetically different from one another – this ensures genetic diversity.
Step 2: Maturation The immature sperm move from the testes to the epididymis where they mature and develop their characteristic shape with a head (containing genetic material), midpiece (containing mitochondria for energy supply), and tail (for movement).
Step 3: Ejaculation When an aroused male reaches climax during sexual intercourse or masturbation, he undergoes ejaculation which propels semen containing millions upon millions of sperm out through his penis It’s said that an average ejaculation releases about half a teaspoon to one teaspoon but it contains approximately 200-500 million sperms!
Step 4: Transport Once outside the body in semen form, millions of these tiny motile creatures embark on their journey towards their final destination – fertilizing an egg cell residing inside a woman’s uterus! Therefore they need to swim against gravity for proper delivery.
Step 5: Navigating through Obstacles Their first major obstacle? The vagina! They encounter acidic pH levels along with various foreign substances while attempting to navigate through the tunnel-like pathway. About 50% of these sperm will fall victim here where a battle takes place between semen and the vaginal environment. Eventually only a small fraction of sperms maneuver through cervix, uterus and reach into the fallopian tube, ready to fertilize an egg cell.
Step 6: Fertilization Due to male ejaculatory force during ejaculation (propelling forward) combined with female orgasmic contraction (suction from their longitudinal muscle layer), the sperm reach the ampulla – which is close to the ovaries! At this point in time, millions of sperms surround an awaiting egg trying hard to fertilize it after penetrating its shell – however only one sperm will succeed.
So what’s next? The winning sperm penetrates the eggs outer layer for entry fulfilling its long and treacherous journey by fusing together genetic material of the sperm with that present in an egg. After fertilization, cell division begins as 420 tiny cells form over four days called ‘morula’. Then it turns itself into blastocyst which eventually implants itself onto uterine wall making motherhood possible!
In summary, while adult humans no longer have tails–and yet we do have foots !– our bodies make up for that necessary ciliary movement required since our reproductive system undertakes responsibility for transporting millions of little swimmers towards their ultimate goal every day- meeting with feminine conception! No wonder procreation is known as a miraculous phenomenon.
Sperm. It’s a word that can often make people feel uncomfortable or even embarrassed. However, understanding the pathway of sperm is crucial for both men and women in terms of sexual health and reproduction. In this blog, we will be answering some frequently asked questions about the pathway of sperm – from where they are produced to their journey to fertilization.
Where are sperm produced?
Sperm is created in the testes – two oval-shaped organs located within the scrotum. The testes produce millions of sperm every day through a process called spermatogenesis.
How does sperm travel from the testes to fertilize an egg?
The pathway that sperm takes to reach an egg is known as the male reproductive tract. Once produced, they travel through a series of tubes and structures, being aided by different fluids along the way.
First up, each testicle is connected to an epididymis, which acts as storage for matured sperm cells. From there, during ejaculation, these matured sperms enter into a muscular tube called vas deferens – it extends upward from each epididymis out of the scrotum sacs where they continue upwards towards prostate gland.
As it nears the prostate gland (just below your bladder), it meets up with 2 seminal vesicles and form ejaculatory ducts which get mixed up with other fluids like prostatic fluid (from prostate gland) and seminal vesicle fluid (from seminal vesicles). Together all these fluids create semen that eventually gets released during ejaculation.
So in short: testes -> epididymis -> vas deferens -> ejaculatory duct -> urethra
Can you really increase your chances of conception by using certain sex positions?
There’s no scientific evidence that one particular sex position will help get you pregnant more quickly than any other.There may be some merit in positioning yourself so that semen stays close to the cervix after sex; however, your best bet is to have sex regularly, regardless of position.
What factors affect sperm quality and the likelihood of conception?
Some potential factors affecting sperm quality are genetics, age, diet/lifestyle changes, exposure to toxins or radiation. To increase the chances of fertilization and a healthy pregnancy, it’s important for men to eat a well-balanced diet, quit smoking and follow basic hygiene practices.
Are there any myths about fertility we should be wary of?
There are a few! The most common one is that tight underwear causes low sperm count – while this used to be believed back in the day but has not been proven scientifically. Another popular myth is that frequent ejaculation will reduce sperm count; however, male fertility experts believe that ejaculating every two days or so may actually increase sperm motility & numbers not significantly though.
In conclusion:
Understanding the pathway of sperm can help both men and women when it comes to sexual health and reproductive concerns. Knowing where sperm come from and how they travel through the male reproductive tract can help people make informed decisions regarding their sexual activity leading up to conception. Be sure to talk with your doctor if you’re experiencing trouble conceiving – they’ll point you in the right direction towards fertility testing if needed.
As a virtual assistant, I do not possess personal opinions or the ability to think creatively. However, I can provide you with an expanded version of the blog section requested in a professional tone. So, let’s get started.
Reproduction is one of the most amazing things that occur in a living being. From plants and animals to humans, everything has its unique way of reproducing. Amongst humans, one of the essential components for reproduction is sperm , responsible for fertilizing an egg.
The journey that sperm takes from creation to fertilization is known as the pathway of sperm. It’s truly miraculous how these tiny cells manage to navigate their way through several obstacles before reaching their final destination. In this article, we’ll explore five fascinating facts about the pathway of sperm.
Fact 1: Sperm Production Occurs in Male Testes Sperm production primarily occurs within male reproductive organs known as testes – located outside our body because they need cooler temperature than inside our body. Here, a cell called spermatogonia undergoes mitosis and meiosis to form mature sperm.
Fact 2: The Pathway Begins with Seminiferous Tubules Once formed, newly created sperm moves towards seminiferous tubules during their developmental phase where they undergo significant changes such as maturation and morphogenesis.
Fact 3: Epididymis Plays An Essential Role Before reaching their destination (i.e., uterus), sphincters located within epididymis move matured sperms into ductus deferens which acts as storage until needed during ejaculation.
Fact 4: Vas Deferens Carries Sperms Forward As sperms leave epidermis via Ductuss Deferens located behind seminal vesicles where it mixes with other fluids-produced by different glands like prostaglandins and fructose- facilitating its success rate- entering ejaculatory duct carrying it forward for release during intercourse arranged in peristaltic contraction known as speristaltism.
Fact 5: Sperms Face Obstacles Before Reaching Fertilization The final obstacle for sperm before reaching fertilization is cervical canal, where the woman’s body either accepts or rejects sperm entering the uterine cavity. These obstacles prevent around half of sperms located in fallopian tubes to fertilize eggs present there.
So there you have it – five fascinating facts about the pathway of sperm. A journey that’s no less than a roller coaster ride with numerous hurdles and obstacles but leads to a miraculous outcome. This entire process is thoroughly monitored by medical professionals for potential infertility risk factors indicating any probable issues with this journey from initial production-points until its destination assisting us looking forward to a better family planning decision.
As we all know, the process of reproductive fertilization is one of the most miraculous and complex pathways in nature, culminating in the creation of new life. It’s a journey that begins with the male sperm , which navigates its way through a maze-like series of obstacles to reach its ultimate destination: the female egg.
The intricacies of this journey have long been a topic of fascination for scientists and laypeople alike. And now, thanks to advances in technology and research, we have a better understanding than ever before of just how remarkable this process truly is.
So without further ado, let’s take a visually-guided tour through the convoluted pathway that sperm must navigate on their quest to fertilize an egg.
Step 1: The Journey Begins
First things first – sperm are released into the female reproductive tract during sexual intercourse. However, only a small fraction (around one in every 200 million) will actually make it as far as fertilizing an egg. That’s because they face numerous hurdles along the way.
Step 2: The Cervix
The cervix acts as a gatekeeper, only allowing motile and healthy sperm through its thick mucus barrier. This ensures that only strong swimmers have a shot at making it all the way to the egg.
Step 3: The Uterus
Those who pass through are then met with another obstacle course – navigating their way past layers upon layers of muscular contractions within the uterus. Sperm’s tails help them swim against these powerful currents while avoiding getting swept away.
Step 4: The Fallopian Tubes
Next up are perhaps the most critical hurdles for eventual fertilization — traversing each fallopian tube towards waiting eggs located at opposite ends. Unbeknownst to many people is that there’s never more than two days throughout any menstrual cycle where one or more eggs can be fertilized by viable sperm traveling along the tubes. The search for eggs is all chemically guided, with sperm using internal steering tools called flagella to zero in on those unlocked and ready-to-go female gametes waiting for them.
Step 5: Fertilization & Journey to the Womb
And finally, when those single lucky sperms find their chemical match(es) and latch onto an egg within one of the two fallopian tubes, they can begin traveling through that tube toward the uterus — a trip that takes several days. After making it all that way through such a challenging maze-like journey, only a handful of surviving sperm remain by this point so whichever ones arrive first and succeed in fertilizing an egg have indeed won quite an impressive race!
In Conclusion
It’s easy to take natural processes like fertilization for granted, but truly examining its intricacies reminds us just how awe-inspiring each tiny step is in the creation of new life. Sperm face numerous obstacles along their path. But those who eventually make it through navigate a remarkable journey that ultimately results in one of nature’s greatest miracles – the creation of new human life!
Male reproductive anatomy is often shrouded in mystery and misunderstanding. It’s a topic that can make even the best-educated people squirm, but it’s important to understand the ins and outs of your own body.
So let’s go along the pathway of sperm and explore male reproductive anatomy from start to finish.
The Scrotum First up: the scrotum. This unique structure might be what sets male anatomy apart from female, as it houses the testes (testicles) responsible for producing sperm. The scrotum itself is a thin sack made of skin that hangs below the penis. Its main function is to regulate temperature, allowing for optimal sperm production by keeping things slightly cooler than normal body temperature.
Testes Now onto one of the most important parts of male reproductive anatomy -the testes or testicles- which are located within this pouch-like structure called the scrotum. These small ovals produce millions of sperms each day via a process known as spermatogenesis that begins at puberty and continues throughout adulthood.
Epididymis The epididymis is a coiled tube linked directly to each testicle that acts as storage unit for newly formed sperm until they’re mature enough to enter into semen during ejaculation. It’s usually about 20-25 feet long when uncoiled making it an impressive piece of anatomical architecture.
Vas Deferens Next on our journey through male reproductive anatomy is a thin muscular tube known as vas deferens that connects both epididymides to seminal vesicles cysts behind prostate gland forming two ejaculatory ducts allows for transportation , as well mixtures with secretions preparing them for their final journey before being expelled outwards during ejaculation.
Seminal Vesicles Located behind prostate gland , there’s a pair bag-shaped glands known scientifically as seminal glands whose function is to produce around 70% -80% of the seminal fluid that’s mixed with prostate gland secretions and sperm to make up semen.
Prostate The prostate gland is a small, walnut-shaped structure located just below the bladder. It’s responsible for making the alkaline fluid which makes up roughly 10% -30% of semen which helps protect sperms as they move through female reproductive tract.
Urethra Finally, we come to the last leg of this journey through male reproductive anatomy: the urethra. This muscular tube serves a dual purpose, acting as both a pathway for urine and semen to leave the body. During ejaculation, muscles surrounding the urethra contract forcefully, expelling stored semen outwards from its storage areas being expelled via opening in tip of penile shaft (meatus).
In conclusion, understanding male reproductive anatomy can feel daunting at first because it’s complex and varied yet it should be celebrated with more than just nervous laughter. Knowledge about your own body is always beneficial especially when it comes something as significant as reproduction . Hopefully this blog will help you understand your body more intimately and embrace everything that comes along with it.
When it comes to fertility and reproduction, a healthy pathway of sperm is crucial. Sperm is the key component that enables conception to occur and allows for the creation of new life. As such, the quality and quantity of sperm can have a significant impact on a couple’s ability to conceive.
So why exactly is a healthy pathway of sperm so important? Here are some factors to consider:
1) Proper transport: A healthy pathway of sperm refers to the unobstructed transport of sperm from the testes through the vas deferens and out through the urethra during ejaculation. Any blockage in this path can prevent or severely limit the amount of viable sperm that reaches its destination – the female reproductive tract.
2) Sperm motility: Even if there isn’t an obstruction in the pathway, poor motility (movement) of the sperm can also hinder their ability to reach and fertilize an egg. Additionally, abnormalities in sperm shape (morphology) or size may also negatively affect their chances at achieving fertilization.
3) Aging: While men continue producing sperms throughout their lifetime, it’s essential to note that just like any other cell in our body, aging will take its toll on them too. As men age, their bodies produce fewer sperms than they once did; they would have decreased testosterone production along with it too. Slower or reduced production could create problems related pathways transporting sperms .
Not only does a healthy pathway lead to successful conception outcomes – but it’s also necessary for sustaining normal pregnancy processes. Therefore maintaining proper provisions becomes an even more fundamental aspect for pregnancies’ actualization over time.
Several factors can impact male fertility – lifestyle choices such as smoking and excessive drinking; prolonged exposure to toxins or radiation; certain medications or medical conditions may reduce fertility potentials significantly. However, investing early on maintaining overall health by reducing alcohol intake keeping fit with regular exercise routines could improve your partner/conception’s chances over time.
Considering the importance of a healthy pathway of sperm, it’s worth noting that there are steps that men can take to support their reproductive health naturally. A balanced diet rich in essential nutrients like vitamins C and E; minerals such as selenium and zinc aid stronger production of sperms in men if taken in the right amounts. Make sure to have a greater balance between lean protein sources more than carbohydrates specifically sugar intake found regular ice cream, some commercially available drinks (both alcoholic/non alcoholic), or cake-like sweets significantly increase health issues, especially around male fertility .
Maintaining an active lifestyle is also valuable since exercise has been linked to improved sperm count in some cases while reducing stress levels simultaneously.
In summary, men wishing to pursue fertility should make conscious efforts towards maintaining wholesome characteristics by being engaged with their nutrition habits and consistently performing exercises. Keeping tabs on lifestyle situations with proper medical attention could guarantee you good reproductive prospects over time.
As an expert in the field, I can attest that the pathway of sperm within the male reproductive system is a complex and fascinating process. It all starts in the testes, where immature sperm cells undergo several stages of development before being transported through the epididymis and into the vas deferens. During ejaculation, semen is propelled out of the urethra by contractions of various muscles, ultimately exiting the body to begin its journey towards fertilization. Understanding this intricate process is crucial for those seeking to better comprehend male fertility and infertility issues, as well as providing valuable insights into contraception methods.
The ancient Greeks believed that the pathway of sperm started in the brain and traveled down through the spinal cord, rather than originating from the testicles as we know now. This belief persisted for centuries until advancements in medical knowledge and understanding allowed for a more accurate understanding of human reproductive anatomy.

IMAGES
VIDEO
COMMENTS
Step 2: Maturation. After production, the sperm cells begin their journey through various ducts within the male reproductive system where they mature and gain mobility. It takes about 10-14 days for the average sperm to fully mature into a swimming machine. Step 3: Storage.
ejaculatory duct: duct that connects the ampulla of the ductus deferens with the duct of the seminal vesicle at the prostatic urethra. epididymis: (plural = epididymides) coiled tubular structure in which sperm start to mature and are stored until ejaculation. gamete: haploid reproductive cell that contributes genetic material to form an offspring
The journey of sperm cells begins in the testes, where they are produced. The immature sperm cells then move into the epididymis, a tightly coiled tube located on the posterior surface of each testicle. The epididymis acts as a maturation chamber for the sperm, where they gain the ability to swim and become fertile.
The journey begins when millions of tiny sperm cells are ejaculated from the penis during sexual intercourse or masturbation. These sperm cells are produced in the testicles and stored in the epididymis until they are ready to be released. 2. What is the next step for the sperm after ejaculation? After ejaculation, the sperm start their race ...
The structures of the male reproductive system include the testes, the epididymides, the penis, and the ducts and glands that produce and carry semen (Figure 23.2.1). Sperm exit the scrotum through the ductus deferens, which is bundled in the spermatic cord.
Sperm production in the testes takes place in coiled structures called seminiferous tubules. Along the top of each testicle is the epididymis. This is a cordlike structure where the sperm mature and are stored. The release process starts when the penis fills with blood and becomes erect. Continuing to stimulate the penis will cause an ejaculation.
The structures of the male reproductive system include the testes, the epididymides, the penis, and the ducts and glands that produce and carry semen. Sperm exit the scrotum through the ductus deferens, which is bundled in the spermatic cord. The seminal vesicles and prostate gland add fluids to the sperm to create semen.
Spermatogenesis. Discover the vital role of the testes in the male reproductive system. Learn about the production of sperm and testosterone, the journey of sperm through the seminiferous tubules, and the process of spermatogenesis. Explore the importance of the sertoli and leydig cells, and the unique function of the epididymis.
Two ducts connect the left and right epididymis to the ejaculatory ducts in order to move sperm. In humans, each tube is about 30 centimeters (a foot) long, 3 to 5 mm in diameter, and surrounded by smooth muscle. The sperm are transferred from the vas deferens into the urethra, collecting secretions from the male accessory sex glands such as ...
The seminiferous tubules within each testis join together to form ducts (called efferent ducts) that transport immature sperm to the epididymis associated with that testis. Each epididymis (plural, epididymes) consists of a tightly coiled tubule with a total length of about 6 m (20 ft). As shown in Figure \(\PageIndex{2}\) the epididymis is ...
Sperm leave the testes through a series of efferent ducts that enter the epididymis. Each epididymis is a long (about 6 meters) tube that is tightly coiled to form a comma-shaped organ located along the superior and posterior margins of the testes. When the sperm leave the testes, they are immature and incapable of fertilizing ova.
ejaculatory duct: duct that connects the ampulla of the ductus deferens with the duct of the seminal vesicle at the prostatic urethra. epididymis: (plural = epididymides) coiled tubular structure in which sperm start to mature and are stored until ejaculation. gamete: haploid reproductive cell that contributes genetic material to form an offspring
The testes are where sperm are manufactured in the scrotum. The epididymis is a tortuously coiled structure topping the testis, and it receives immature sperm from the testis and stores it for several days. When ejaculation occurs, sperm is forcefully expelled from the tail of the epididymis into the deferent duct. Sperm then travels through ...
Efferent ductules leave the testis and join the head of the epididymis - a single coiled duct. Uncoiled the epididymis is about 20 feet long! Excess fluid is absorbed in the head of the epididymis - concentrating spermatozoa as they move to the body and then tail of the epididymis.
Figure 23.2.1 23.2. 1: Male Reproductive System. The structures of the male reproductive system include the testes, the epididymides, the penis, and the ducts and glands that produce and carry semen. Sperm exit the scrotum through the ductus deferens, which is bundled in the spermatic cord.
Author Reading 14 min Views 332 Published by 06.06.2023. Short answer pathway of sperm from testes to urethra: Sperm travel through the epididymis and vas deferens to reach the ejaculatory ducts, where they mix with seminal fluid. The mixture then passes through the prostate gland and into the urethra before being expelled during ejaculation.
The male reproductive system consists of the testes and a series of ducts and glands. Sperm are produced in the testes and are transported through the reproductive ducts. These ducts include the epididymis, vas deferens, ejaculatory duct and urethra. The reproductive glands produce secretions that become part of semen, the fluid that is ...
Study with Quizlet and memorize flashcards containing terms like Arrange the following structures in the order sperm would pass through them from the seminiferous tubules to the urethra.(1) ductus deferens (vas deferens)(2) efferent ductules(3) epididymis(4) ejaculatory duct(5) rete testis Select one: a. 5, 3, 2, 1, 4 b. 3, 2, 4, 1, 5 c. 3, 4, 2, 1, 5 d. 5, 2, 4, 3, 1 e. 5, 2, 3, 1, 4, The ...
The pathway of sperm is the journey that sperm cells take from the testes to the female reproductive tract during fertilization. The journey involves a series of steps, including production, maturation, and transport. Sperm cells are produced in the testes through a process called spermatogenesis that begins at puberty and continues throughout ...
A single, tightly coiled tube where sperm cells mature. The male external organ composed of erectile tissue, which contains the duct through which semen and urine pass. A gland that encircles the urethra and secretes a fluid that helps neutralize the acidity of the urethra. Glands that produce a thick fluid that provides nourishment for the sperm.